Breast cancer risk
We recognise that the orthopaedic community have diverse gender identities.
Here, we use the terms female and male to refer to biological sex, in line with the scientific literature relating to breast cancer.
1. Incidence and risk factors
Breast cancer is the most common female cancer in the UK, and the second highest cause of female cancer mortality, accounting for 11,000 deaths per year.
Women in the UK have a 1 in 7 lifetime risk of breast cancer. The overall cancer incidence has increased since the 1990s, with the highest increases seen in the working age population. Breast cancer now accounts for 43% of cancer cases in women aged 25-49 years [15].
Many breast cancer risk factors are not modifiable, and include increasing age and genetic predisposition. However, 23% of breast cancer cases are deemed preventable, with 1% attributable to ionising radiation [15,16]. The IARC have defined ionising radiation as having 'sufficient' and 'convincing' evidence as a breast cancer risk factor.
Female breast tissue extends into the axilla and the majority of breast cancers occur in the upper outer quadrant (UOQ) [17].
2. Risk in orthopaedic surgeons
The current risk of breast cancer in orthopaedic surgeons is unknown. As the proportion of female orthopaedic surgeons increases, we must continue to collect data to clarify whether an additional risk of breast cancer exists. There have been no reports of an increased risk in male surgeons, as they have no breast tissue extending into the axilla [18].
Two self-reported US studies of female orthopaedic surgeons have shown a 1.9 fold increase in all-cause cancer incidence and a 2.9-3.9 fold increased incidence of breast cancer. This increase was not seen in plastic surgeons or urologists, and remained when the cohort was matched against a control population [8-10].
Occupational radiation exposure has been associated with increased prevalence of female breast cancer in other healthcare cohorts, including US radiology technicians, Chinese radiographers, and Finnish doctors [5,19,20].
3. Current PPE and effectiveness
Currently available PPE consists of tabard-style one-piece gowns or a two-piece skirt and vest. Simulated studies measuring dose exposure to the UOQ of the breast have shown that these provide inadequate protection, particularly with the C-arm in the lateral position, and the surgeon standing perpendicular to the table [21].
Dosimeters worn over these gowns showed the area next to the axilla and UOQ received the highest dose of radiation in the torso [22].
Studying different designs in a simulated setting showed no reduction in radiation exposure to the UOQ and axilla in a standard tabard gown when compared to no gown. A significant reduction could be achieved with the use of sleeves or axillary shields [23].
Provision of axillary and UOQ coverage has traditionally involved custom-made designs, using sleeves or axillary shields. Axillary wings have been promoted in the USA, but a previously tested type has not been shown to reduce axillary exposure in simulated settings [23].
4. Breast and axillary protection for the female orthopaedic surgeon
Current options in the UK
To date, the only way to obtain axillary and full breast protection to include the UOQ is with individual custom-made gown designs. A team has been working with partners in industry to develop and produce a design that is comfortable for female orthopaedic surgeons, covers the lateral chest wall and axilla, and provides protection for the axillary tail and UOQ of the breast whilst remaining functional for the demands of orthopaedic surgery.
Early testing has occurred on a range of options to provide improved protection. The aim is to develop a commercially available option that does not require custom fitting, and can therefore be made available to all female surgeons.
i) Focus on reducing individual exposure
The most important protection from radiation comes from reducing individual exposure as per the guidance on the previous page, Occupational radiation exposure risk in orthopaedics.
For maximal breast protection, please ensure that all surgical team members:
- Stand as far back from the source as possible
- Keep arms by side where able
- Stand square to the source to avoid exposing the axilla
- Reduce the use of direct lateral views
ii) Lead protection garments in widespread current use

Evidence from the US [23] and from provisional testing here has shown that standard tabard gowns do not protect the breast or axilla from radiation. Increased coverage results in reduction in dose, and so vest tops should be well-fitted to the individual and as close to the axilla as possible.
We recommend:
- Female orthopaedic surgeons should not be using tabard gowns
- Vests should be fitted to the size of the individual and as close to the axilla as possible
- Minimum lead thickness should be 0.25mm
- Detachable sleeves are not recommended
iii) Breast protection options
A number of options are available for breast and axillary protection in the UK. These are in different stages of development and availability at present. Examples are given below, including the names of companies associated with different products.
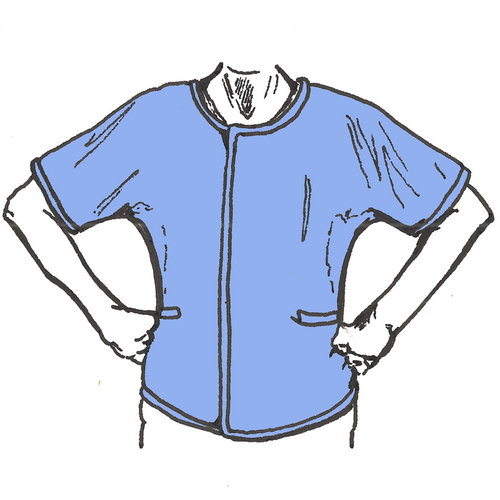
Vest with sleeves
This is a fully integrated top with sleeves protecting the front and back of the axilla (Made by ProtecX, UK).

Vest with wings
Integrated wings on a well-fitted vest. The additional material fans out over the front of the axilla, but does not extend to the back. (Made by Infab, USA; UK distribution via Platform 14).

Vest with axillary shields
A detachable shield which encircles the axilla that can we worn with any apron (as it doesn’t require any retrofitting or adjustment to an existing apron). (Made by Rothband, UK).
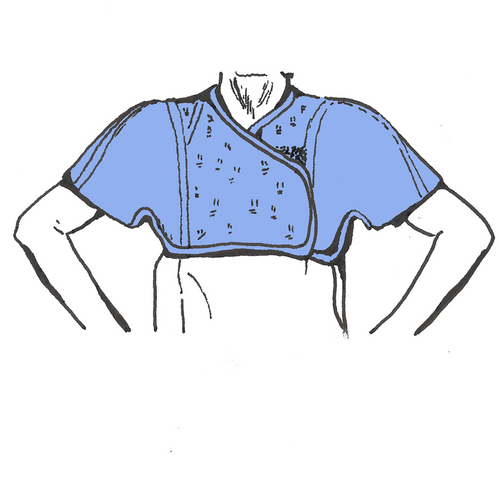
Bolero
Lead sleeves with a lightweight mesh across front and back which can be worn under a standard vest. (Made by ProtecX, UK and Mavig, Germany).
iv) Future research
Preliminary trials have been performed in a simulated setting to quantify breast and axillary tail exposure with different gown types. These have shown a marked difference between any axillary coverage and standard gowns, but there is insufficient evidence at present to recommend one specific type of axillary protection over another.
Further work in this area remains ongoing.
The BOA would support a formal study if one was proposed.
v) Choosing a gown
Surgeons looking to purchase a garment for individual use should ensure:
- A good, close fit
- Comfortable and free movement of the arms
- Axillary and breast cover are maintained with the arm abducted
Different body shapes and sizes may require trialling different options to find the best fit.
Companies have been invited to the BOA 2023 in Liverpool to allow surgeons to test products for comfort and coverage.
References
[1] AO. Characteristics of X-rays [Internet]. [cited 2023 Feb 4]. Available from: https://images.aofoundation.org/CIP/asset/download/Gallery/13464
[2] Raza M, Geleit R, Houston J, Williams R, Trompeter A. Radiation in orthopaedics (RIO) study: a national survey of UK orthopaedic surgeons. BJR. 2021 Sep 1;94(1125):20210736.
[3] Radiation protection of medical staff in orthopedic surgery | IAEA [Internet]. [cited 2022 Nov 9]. Available from: https://www.iaea.org/resources/rpop/health-professionals/other-specialities-and-imaging-modalities/orthopedic-surgery/staff#5
[4] Laurier D, Richardson DB, Cardis E, Daniels RD, Gillies M, O'Hagan J, et al. The International Nuclear Workers Study (Inworks): A Collaborative Epidemiological Study to Improve Knowledge About Health Effects of Protracted Low-Dose Exposure. Radiat. Prot. Dosim. 2017. Apr, 173, https://doi.org/10.1093/rpd/ncw314
[5] Sigurdson AJ, Doody MM, Rao RS, Freedman DM, Alexander BH, Hauptmann M, et al. Cancer incidence in the US radiologic technologists health study, 1983-1998. Cancer. 2003 Jun 15;97(12):3080–9.
[6] Roguin A, Goldstein J, Bar O, Goldstein JA. Brain and neck tumors among physicians performing interventional procedures. Am J Cardiol. 2013 May 1;111(9):1368–72.
[7] Ramoutar DN, Thakur Y, Batta V, Chung V, Liu D, Guy P. Orthopaedic Surgeon Brain Radiation During Fluoroscopy: A Cadaver Model. J Bone Joint Surg Am. 2020 Nov 18;102(22):e125.
[8] Chou LB, Johnson B, Shapiro LM, Pun S, Cannada LK, Chen AF, et al. Increased Prevalence of Breast and All-cause Cancer in Female Orthopaedic Surgeons. JAAOS Glob Res Rev [Internet]. 2022 May [cited 2022 Oct 31];6(5). Available from: https://journals.lww.com/10.5435/JAAOSGlobal-D-22-00031
[9] Chou LB, Chandran S, Harris AHS, Tung J, Butler LM. Increased Breast Cancer Prevalence Among Female Orthopedic Surgeons. Journal of Women’s Health. 2012 Jun;21(6):683–9.
[10] Chou LB, Lerner LB, Harris AHS, Brandon AJ, Girod S, Butler LM. Cancer Prevalence among a Cross-sectional Survey of Female Orthopedic, Urology, and Plastic Surgeons in the United States. Women’s Health Issues. 2015 Sep;25(5):476–81.
[11] Patra SK, Shetty AP, Jayaramaraju D, Rajasekaran S. Radiation Exposure to the Surgeon, Surgical Assistant, and Scrub Nurse During Closed Intramedullary Nailing of Long Bones-Does It Vary Depending on the Experience of the Surgeon? J Orthop Trauma. 2019 Feb;33(2):e52–7.
[12] Patel N, Mohamed A, Cooper G, McFadyen I. Ionising radiation exposure in paediatric trauma. annals. 2014 Apr;96(3):190–3.
[13] Quah C, Mehta R, Shivji F, Hassan S, Chandrasenan J, Moran C, et al. The effect of surgical experience on the amount of radiation exposure from fluoroscopy during dynamic hip screw fixation. annals. 2017 Mar;99(3):198–202.
[14] Malik AT, Rai HH, Lakdawala RH, Noordin S. Does surgeon experience influence the amount of radiation exposure during orthopedic procedures? A systematic review. Orthop Rev (Pavia) [Internet]. 2019 Mar 12 [cited 2022 Oct 31];11(1). Available from: https://www.pagepress.org/journals/index.php/or/article/view/7667
[15] Cancer Research UK. Internet. [cited 2023 Feb 8] Available from: https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/breast-cancer.
[16] Ronckers CM, Erdmann CA, Land CE. Radiation and breast cancer: a review of current evidence. Breast Cancer Res. 2004 Feb;7(1):21.
[17] Rummel S. Tumour location within the breast: Does tumour site have prognostic ability? ecancer [Internet]. 2015 Jul 13 [cited 2022 Nov 7];9. Available from: http://www.ecancer.org/journal/9/full/552-tumour-location-within-the-breast-does-tumour-site-have-prognostic-ability.php
[18] Swergold N, Murthy V, Chamberlain RS. Males at High Risk for Breast Cancer: Who Are They and How Should We Screen Them? SS. 2014;05(07):320–31.
[19] Wang JX, Zhang LA, Li BX, Zhao YC, Wang ZQ, Zhang JY, et al. Cancer incidence and risk estimation among medical x-ray workers in China, 1950-1995. Health Phys. 2002 Apr;82(4):455–66.
[20] Jartti P, Pukkala E, Uitti J, Auvinen A. Cancer incidence among physicians occupationally exposed to ionizing radiation in Finland. Scand J Work Environ Health. 2006 Oct;32(5):368–73.
[21] Valone LC, Chambers M, Lattanza L, James MA. Breast Radiation Exposure in Female Orthopaedic Surgeons. The Journal of Bone and Joint Surgery. 2016 Nov 2;98(21):1808–13.
[22] Hurley RJ, McCabe FJ, Turley L, Maguire D, Lucey J, Hurson CJ. Whole-body radiation exposure in Trauma and Orthopaedic surgery. Bone & Joint Open. 2022 Nov 1;3(11):907–12.
[23] Van Nortwick SS, Leonard DA, Finlay AK, Chou L, Valone LC. Methods for Reducing Intraoperative Breast Radiation Exposure of Orthopaedic Surgeons. Journal of Bone and Joint Surgery. 2021 Sep 1;103(17):1646–51.
