BOAST - Open Fractures



Date Published: December 2017
Last Updated: December 2017
Background and justification
Open fractures may require timely multidisciplinary management. The consequences of infection, can be great both for the individual patient and the community. Trauma networks and hospitals require the appropriate pathways and infrastructure, to manage these patients, to enable optimum recovery and to minimise the risk of infection.
Inclusions:
All patients with open fractures of long bones, hind foot or midfoot (excluding hand, wrist, forefoot or digit).
Standards for Practice
- Patients with open fractures of long bones, hind foot or midfoot should be taken directly or transferred to a specialist centre that can provide Orthoplastic* care. Patients with hand, wrist, forefoot or digit injuries may be managed locally following similar principles.
- Intravenous prophylactic antibiotics should be administered as soon as possible, ideally within 1 hour of injury.
- There should be a readily accessible published network guideline for the use of antibiotics in open fractures.
- The examination of the injured limb should include assessment and documentation of the vascular and neurological status. This should be repeated systematically, particularly after reduction manoeuvres or the application of splints. Management of suspected compartment syndrome should follow BOAST guidelines.
- The limb should be re-aligned and splinted.
- Patients presenting with arterial injuries in association with their fracture should be treated in accordance with the BOAST for arterial injuries.
- In patients where an initial “Trauma CT” is indicated there should be protocols to maximise the useful information and minimise delay:
— The initial sequence should include a head to toes scanogram. This should be used with clinical correlation to direct further specific limb sequences during that initial CT examination.
— There should be a local policy on the inclusion of angiography in any extremity CT related to open fractures. - Prior to formal debridement the wound should be handled only to remove gross contamination and to allow photography, then dressed with a saline-soaked gauze and covered with an occlusive film. ‘Mini-washouts’ outside the operating theatre environment are not indicated.
- All trauma networks must have information governance policies in place that enable staff to take, use and store photographs of open fracture wounds for clinical decision-making 24 hours a day.
- Photographs of open fracture wounds should be taken when they are first exposed for clinical care, before debridement and at other key stages of management. These should be kept in the patient’s records.
- The formation of the management plan for fixation and coverage of open fractures and surgery for initial debridement should be undertaken concurrently by consultants in orthopaedic and plastic surgery (a combined orthoplastic approach).
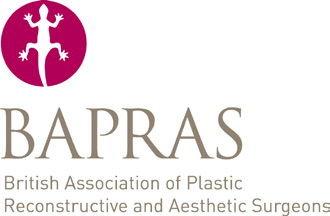
- Debridement should be performed using fasciotomy lines for wound extension where possible (see overleaf for recommended incisions for fasciotomies of the leg)
— Immediately for highly contaminated wounds (agricultural, aquatic, sewage) or when there is an associated vascular compromise (compartment syndrome or arterial disruption producing ischaemia).
— within 12 hours of injury for other solitary high energy open fractures.
— within 24 hours of injury for all other low energy open fractures. - Once debridement is complete any further procedures carried out at that same sitting should be regarded as clean surgery; i.e. there should be fresh instruments and a re-prep and drape of the limb before proceeding.
- Definitive soft tissue closure or coverage should be achieved within 72 hours of injury if it cannot be performed at the time of debridement.
- Definitive internal stabilisation should only be carried out when it can be immediately followed with definitive soft tissue cover.
- When a decision whether to perform limb salvage or delayed primary amputation is indicated, this should be based on a multidisciplinary assessment involving an orthopaedic surgeon, a plastic surgeon, a rehabilitation specialist, the patient and their family or carers.
- When indicated, a delayed primary amputation should be performed within 72 hours of injury.
- Each trauma network should submit appropriate data to the TARN, monitor its performance against national standards and audit its outcomes.
- All patients should receive information regarding expected functional recovery and rehabilitation, including advice about return to normal activities such as work and driving.
*The BAPRAS/BOA group recommend that for clarity the narrative description of an Orthoplastic Service by NICE is broken into its component parts as follows: a combined service of Orthopaedic and Plastic Surgery Consultants; sufficient combined operating lists with consultants from both specialties to meet the standards for timely management of open fractures; scheduled, combined review clinics for severe open fractures; specialist nursing teams able to care for both fractures and flaps. In addition, an effective orthoplastic service will also: submit data on each patient to the national trauma database (TARN) and hold regular clinical audit meetings with both orthopaedic and plastic surgeons present. Please note: the definition of an Orthoplastic Centre was updated in November 2019.
Evidence base:
NICE Complex fracture guideline https://www.nice.org.uk/guidance/NG37/chapter/recommendations
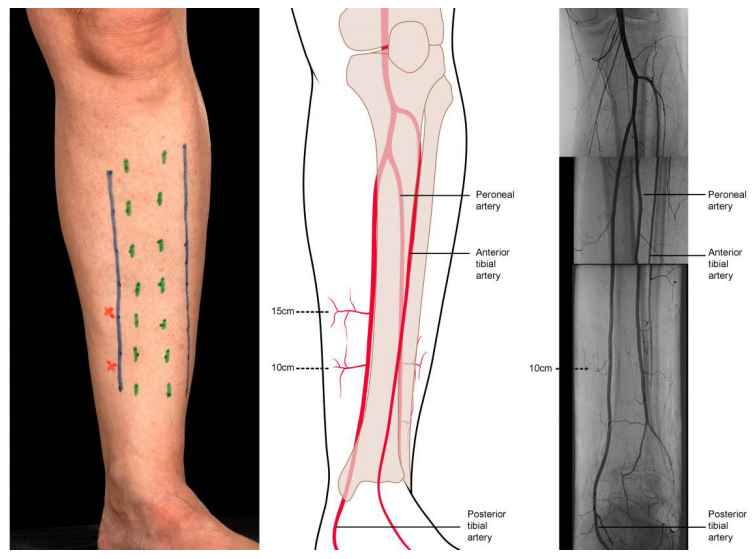
Figure showing recommended incisions for wound debridement and fasciotomies in the leg. The medial incision alone is usually sufficient for debridement and preserves the perforators arising from the posterior tibial vessels, which form the basis of local fasciocutanoeus flaps. It also provides access to the posterior tibial artery and venae commitans when required as recipient vessels for free flaps. The lateral incision is used for decompression of the anterior and peroneal compartments in patients with compartment syndrome. (A) Margins of subcutaneous border of the tibia marked in green, access incisions marked in blue and perforators arising from the medial side as red crosses. (B) Line drawing depicting the location of the perforators, with approximate indicative distances from the tip of the medial malleolus. (C) Montage of arteriogram.
Figure showing cross section through leg showing incisions to decompress all four compartments
