UK Orthopaedic trainees covering medical COVID-19 wards and still meeting Joint Committee on Surgical Training trauma procedure guidelines: A successful multifaceted collaborative model
By David Ferguson, Rory Cuthbert, Edward Karam, Cameron Dott, Lilanthi Wickramarachchi, Asif Parkar, Shivakumar Shankar, Krishna Vemulapalli
Barking, Havering and Redbridge University Hospitals NHS trust
Corresponding author email: [email protected]
Published 04 September 2020
Abstract
Aims: The UK Government’s national lockdown from 23 March 2020 coupled with the British Orthopaedic Association guidance on non-operative management of trauma has reduced trauma operating nationwide during the COVID-19 pandemic. The aim of this study was to determine if despite orthopaedic registrars moving to a COVID-19 rota with medical duties, a multifaceted collaborative approach between trainee orthopaedic registrars could result in a maintenance of trauma theatre activity similar to standard practice levels.
Methods: Electronic logbook data was collected from all participating trainee registrars in the department. Two time periods were determined; a pre COVID-19 baseline equivalent to previous standard 6-month orthopaedic rotation, and a COVID-19 rota period equivalent to the duration of the full UK lockdown.
Results: 2,162 total potential hours of trauma operating under pre COVID-19 rota were compared to 631 hours under COVID-19 rota conditions. Departmental daily mean rate of registrars acquiring the Joint College of Surgical Training (JCST) indicative trauma numbers did not change between pre COVID-19 rota and COVID-19 rota periods (0.26 [0.19-0.38] vs 0.40 [0.15-0.72] p = 0.140). Similarly, the mean rate of registrars acquiring total trauma numbers did not change between the same rota periods (0.37 [0.19-0.49] vs 0.53 [0.15-0.85] p = 0.254).
Conclusion: Through a multifaceted collaborative approach, orthopaedic registrars were able to maintain a constant rate of acquiring indicative and total trauma cases, despite changing work schedules. The number of cases acquired surpassed the yearly JCST requirement for satisfactory Annual Review of Competency Progression (ARCP).
Introduction
Training future surgeons is a foundation of any healthcare system, with both emergency and elective surgery significant factors in contributing to population health1,2. A rapid re-organisation and prioritisation of healthcare delivery was necessitated by the COVID-19 global pandemic, with a minimum 3-month cessation of elective operating, across all 10 UK surgical specialties, from April 20203. Despite a UK Government lockdown commencing on 23 March 20204, Accident and Emergency (A&E) departments in England still received 75% of the attendances of the preceding week5. Even with a complete UK lockdown in April 2020, monthly A&E attendances remained high at 916,5816, with the subsequent need for a dedicated orthopaedic trauma service remaining in most NHS trusts7.
Landmark modelling from Imperial College London provided a stark picture of potential loss of life without swift action8. This data underpinned the UK Government strategy with resultant reallocation of many orthopaedic doctors to support intensive treatment units (ITU), emergency departments and COVID-19 medical ward duties – a move supported by Health Education England9. General Medical Council (GMC) guidance provided reassurance for doctors working beyond the scope of their typical practice – something never before actioned in clinical practice10. UK orthopaedic trainees due to rotate to new subspecialty placement and continue training during the ‘delay phase’ of COVID-19 response were held in post, with a six month addition to the 72-month training programme advised11.
Certain trusts, including our own, reorganised orthopaedic trauma services as part of a coordinated response to increase capacity to care for patients with COVID-1912. This required relocation to a temporary Independent Sector Treatment Centre (ISTC) of a COVID-19 free trauma service providing care for a diverse community of 750,000 people across a 939-bed acute hospital, and 450-bed elective and rehabilitation satellite site. Additionally, all orthopaedic registrars in the department moved to a rolling pattern of 3 days on 3 days off. This involved working for 3 days in either general medical COVID-19 ward cover, day on-call, night on-call or trauma theatres, followed by 3 days rest between each block of work. This response enabled a major contribution to the wider hospital trust COVID-19 response, whilst maintaining a baseline continuity of orthopaedic training. During normal conditions our department runs 88 hours of trauma operating per week split across 22 operating sessions. During the COVID-19 rota period we had 96 hours of trauma operating per week across 24 operating sessions. This marginal rise in the theatre availability was achieved as more theatre capacity was available at the ISTC.
In routine clinical practice at our trust, 12 consultants are paired with 12 associate specialists, and 12 registrars. Most of the registrars are trainees from the North Central and East London rotations. The JCST mandates that as part of the yearly requirements, trainees perform 300 operative cases per year with 70% as first surgeon. Additionally, certain indicative operative procedures together with a minimum acceptable number are set and must be signed off prior to completion of training13. To permit progression, trainees are allocated to a dedicated trauma week 1 in every 12, together with additional lists to comprise a mean of 1.74 +/- 0.23 (1.S.D) trauma sessions per week. At the interim ARCP following October 2019 – April 2020 rotations, all trainees were deemed to have acquired the necessary indicative trauma case numbers and total number of trauma cases to progress to the next six months of training.
Following a new ‘3 on 3 off’ rolling rota with services across two separate sites, a resultant doubling of night and on-call commitments plus a reduction in baseline trauma operating to three days per 30 was implemented. All full-time trainees working during the COVID-19 rota period devised a multifaceted collaborative approach to maximise operative training opportunities, supported by the department’s consultants. Firstly, trainees were encouraged to ‘double scrub’ for each other’s lists. Secondly, when appropriate trainees would step up to fill associate specialist vacancies on the operating lists. Thirdly, for any periods of trainee illness or self-isolation, providing sufficient staffing was present at trust COVID-19 ward cover, the trainee allocated to COVID-19 medical duties would return to orthopaedic theatres.
The purpose of this study was to assess how well trainees were able to collaborate together during a time of national crisis to provide essential COVID-19 duties to one of the busiest trusts in the UK, whilst continuing their orthopaedic trauma training. The null hypothesis was that there was no difference in trauma elogbook caseload for both indicative or total trauma cases between normal rota and COVID-19 rota periods.
Methods
Trainees working for the full duration of the UK lockdown submitted their electronic operative logbooks for analysis. Two distinct periods were chosen; a reference period following trainee rotation from 2 October 2019 – 22 March 2020 (172 days) under normal rota conditions. A second period 23 March 2020 – 8 May 2020 (46 days) was defined, to determine the change in operative activities during the full UK lockdown – coinciding with the rolling COVID-19 rota period.
A pragmatic data analysis approach was employed, reflecting the nature of delivering a constantly available 24/7, 365 day a year trauma service, and training surgeons within such delivery. Rather than adjusting for periods of self-isolation, study and annual leave which were taken during the normal and COVID-19 rota periods, this pragmatic approach reflects the reality of trauma training with the various setbacks which occur within a six year training programme.
All logbooks were anonymised and reviewed independently by two authors (DF, RC). Discrepancies were discussed and a consensus reached. Total indicative trauma cases recorded as either supervised trainer scrubbed (STS) or supervised trainer unscrubbed (STU) were extracted and analysed, together with total trauma cases of any supervision level for both periods (Table 1).
|
|
Normal rota |
COVID-19 rota |
|
|
Total operating hours |
2,162 |
631 |
|
|
Total indicative trauma numbers |
267 |
110 |
|
|
Daily rate of indicative trauma (1.S.D) |
0.26 [0.19-0.38] |
0.40 [0.15-0.72] |
p = 0.140 |
|
Total trauma |
381 |
137 |
|
|
Daily rate of total trauma (1.S.D) |
0.37 [0.19-0.49] |
0.50 [0.15-0.85] |
p = 0.254 |
A daily rate at which both indicative trauma cases and total trauma cases were acquired under the two defined periods were calculated for each trainee, together with departmental mean and range. Normal distribution of data was assumed with paired Students t-test were performed, comparing normal rota with COVID-19 rota periods for both indicative trauma cases and total trauma cases. Statistical significance was set at p ≤ 0.05. Further calculations were performed to determine the daily rate at which trainees are required to obtain both indicative and total trauma numbers to meet JCST, ARCP requirements.
Results
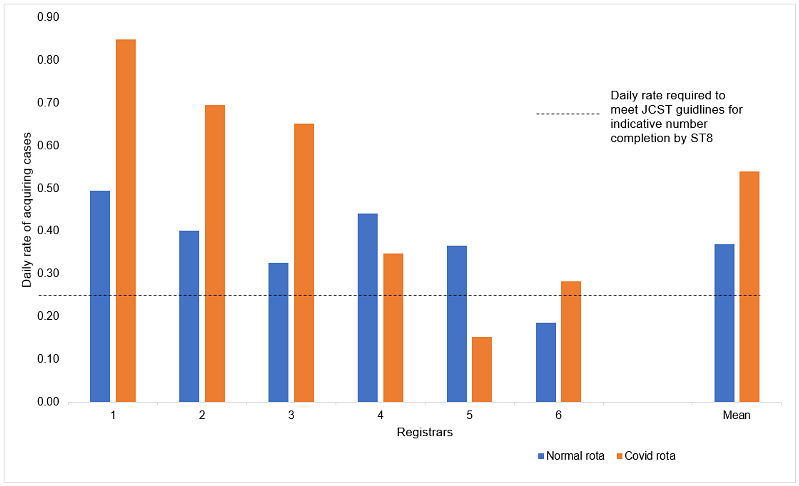
Six of the seven (85.7%) trainee registrars submitted complete electronic logbooks. 2,162 hours of departmental trauma operating time occurred during normal rota conditions, compared to 631 hours under the COVID-19 rota. The departmental mean daily rate of acquiring indicative trauma cases did not vary between normal rota and COVID-19 rota periods 0.26 [range 0.19-0.38] vs 0.40 [range 0.15-0.72] p = 0.140 (Figure 1). Similarly, departmental mean daily rate of acquiring total trauma cases did not vary between normal and COVID-19 rota periods 0.37 [range 0.19-0.49] vs 0.50 [0.15-0.85] p = 0.254 (Figure 2). Totals, together with daily rates of acquiring each of the nine indicative trauma cases during normal and COVID-19 rota periods are available (Table 2).
Figure 1: Comparison of daily rate of acquiring indicative trauma numbers from normal rota to COVID-19 rota
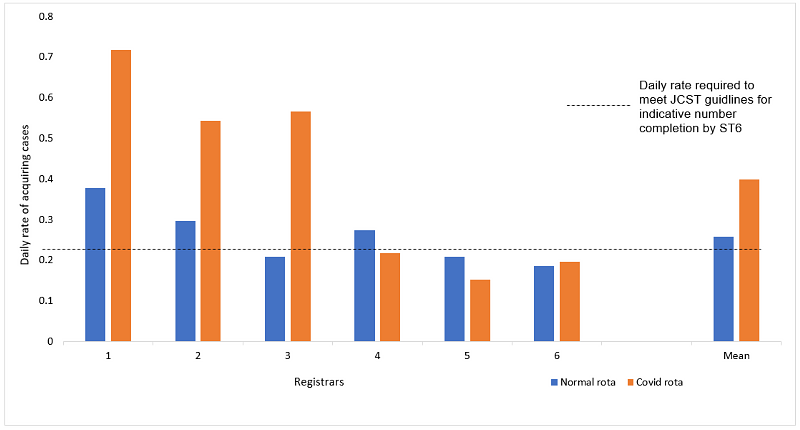
Figure 2: Comparison of daily rate of acquiring total trauma numbers from normal rota to COVID-19 rota
|
|
Normal rota |
Mean daily rate |
COVID-19 rota |
Mean daily rate |
|
Compression hip screw for intertrochanteric fracture neck of femur |
35 |
0.20 |
15 |
0.33 |
|
Hemiarthroplasty for intracapsular neck of femur fracture |
55 |
0.32 |
22 |
0.48 |
|
Application of limb external fixator |
7 |
0.04 |
0 |
0.00 |
|
Tendon repair for trauma |
22 |
0.13 |
6 |
0.13 |
|
Intramedullary nailing including flexible nailing for fracture or arthrodesis |
32 |
0.19 |
32 |
0.70 |
|
Plate fixation for fracture or arthrodesis |
94 |
0.55 |
29 |
0.63 |
|
Tension band wire for fracture or arthrodesis |
6 |
0.03 |
2 |
0.04 |
|
K wire fixation for fracture or arthrodesis |
15 |
0.09 |
1 |
0.02 |
|
Children's displaced supracondylar fracture |
1 |
0.01 |
3 |
0.07 |
|
Total indicative trauma |
267 |
1.55 |
110 |
2.98 |
0.25 indicative trauma cases per day is defined as the threshold required for satisfactory completion of all indicative trauma procedures by end of ST6 – the waypoint at which trainee’s are eligible to apply for the FRCS examination. This threshold was met both under normal rota conditions at a departmental mean 0.26 [range 0.19-0.38] cases per day, and COVID-19 rota at a departmental mean 0.40 [range 0.15-0.72] cases per day (Figure 1). Total trauma cases requires a slightly higher daily rate of 0.27 to achieve competencies by ST8. Under both normal and COVID-19 rota periods this threshold was met at 0.37 [range 0.19-0.49] and 0.50 [range 0.15-0.85] per day respectively (Figure 2).
Discussion
This study demonstrates that despite the global healthcare response to the COVID-19 pandemic and impact on surgical training pathways14, through a collaborative effort amongst trainees it remains possible to support a medical COVID-19 rota, and continue to achieve the same number of trauma cases as under normal working conditions and as necessary for ARCP.
Despite full UK lockdown restrictions as commenced on 23rd March 2020 mandating against all but essential travel4, one multicentre study recently reported that compared to pre COVID-19 incidence, fragility fractures requiring admission remained constant, whilst trauma admissions reduced by 53.7%15. Our trust did not outsource any trauma, but determined a work pattern of keeping a similar hours per week trauma capacity, with the expectation that efficiency would reduce given the necessary personal protective equipment (PPE) precautions to be taken16. This reactive trauma service permitted a titration of the number of theatre sessions running to permit a constant supply for the varying trauma demand.
Our trust is located on the periphery of London with an increased proportion of BME groups. Recent intensive care unit data has been published suggesting over a third of COVID-19 patients are from this demographic17,18. We were the first UK trust reported to have admitted, treated and discharged over 1,000 COVID-19 patients, indicating the rapid response and healthcare worker role redeployment required to deliver the necessary care19. Multiple informal discussions were held between the registrars after a review of the number of pending trauma cases requiring operative management. This resulted in the multifaceted collaborative model evolving in an effort to maintain exposure to training cases during the COVID-19 rota. Work schedules changed from a standard 46¾ hours per week to department wide COVID-19 support rota of 45½ hours per week. Under the new rota a work pattern of three 12-hour days followed by three days off resulted in considerably more zero days and coalesced to enable the model to work.
Firstly, registrars designated to trauma theatres opened opportunities for their colleagues to join their lists, ‘double scrubbing’ to enhance operative exposure. This was made possible by a rota with three days of no clinical contact, meaning that once a registrar had had sufficient rest, they could choose to use their free time to join their colleagues. ‘Double scrubbing’ has recently been encouraged in guidance by the British Orthopaedic Association in the restarting of non-urgent trauma cases, as a preventative measure against deskilling20. The process of two registrars operating had a requirement for PPE to be available and also for consultant supervision of all cases. Registrars would share anonymised details of pending trauma via messaging services to determine trauma caseload and number of anticipated surgeons the next day, thus prioritising patient and operative safety whilst continuing to accrue trauma exposure.
Secondly, our department’s model of having an associate specialist present to cover all operating lists provided further scope for registrars to attend theatre. Given the experience of associate specialists, there is no yearly requirement of indicative numbers or total operative numbers as with trainee registrars. Knowledge of the trainees’ requirement to obtain a satisfactory caseload number, and providing suitable operative abilities, associate specialists would opt not to scrub yet be available in theatre premises for supervision when safe. This was determined on a case by case basis where appropriate and resulted in increased operative exposure.
Thirdly, during periods of sickness or self-isolation, providing there was a sufficient number of trust doctors to staff the general medical COVID-19 rota, orthopaedic registrars were reassigned from COVID-19 duties to support trauma theatre workload. Given the reactive nature of the COVID-19 rota and cessation of all elective surgery and routine medical outpatients clinics, there were regular periods of sufficient staffing to permit release of an orthopaedic registrar. Delivery of this was through consultant leads who would be in contact multiple times per day with registrars and COVID-19 rota managers to ensure appropriate allocation of workforce for maximal efficiency. Through this multifaceted approach, maintenance of the same trauma operative exposure as under normal rota conditions was possible.
There are a few limitations to this paper. As a single centre study, it is not reflective of practice across all UK trusts. A relatively small sampling time frame of 46 days during lockdown introduces the risk of sampling bias. In hospitals reorganising as COVID-19 only sites during the pandemic with outsourcing of trauma workload, implementation of this model is not possible. No adjustment was made for periods of self-isolation or sick leave. Finally, successful implementation of this model requires a cohort of registrars who are all able to work collaboratively and share learning opportunities whilst having sufficient operative ability to manage basic trauma with a consultant present but unscrubbed in theatre.
Conclusions
We demonstrate a multifaceted model of collaboration between orthopaedic registrars to permit constant achievement of baseline trauma numbers needed for ARCP. Despite moving to a rota resulting in double the number of nights and on calls and periods of dedicated COVID-19 medical ward support, through this approach registrars were able to support each other’s training and maximise theatre opportunities. No difference in trauma theatre cases existed during the normal rota compared to full UK lockdown COVID-19 rota period. This level of operative exposure may be sufficient in certain circumstances to enable trainees to progress as planned through training with no additional time required. Whilst we all strive to ensure that the global healthcare COVID-19 response remains a once in a generation event, should a similar situation arise in the future, this model may represent a framework for safe rota management of orthopaedic trainees in the appropriate setting.
References
- Brindle ME, Gawande A. Managing COVID-19 in Surgical Systems. Ann Surg. 2020;272(1):e1-e2.
- McQueen KAK, Ozgediz D, Riviello R, Hsia RY, Jayaraman S, Sulliavan SR, Meara JG. et al. Essential surgery: Integral to the right to health. Health Hum Rights. 2010;12(1):137-52.
- Iacobucci G. Covid-19: all non-urgent elective surgery is suspended for at least three months in England. BMJ. 2020;368:m1106.
- Department of Health (2020). Prime Minister's statement on coronavirus (COVID-19): 23 March 2020. Available at: https://www.gov.uk/government/speeches/pm-address-to-the-nation-on-coronavirus-23-march-2020.
- Thornton J. Covid-19: A&E visits in England fall by 25% in week after lockdown. BMJ. 2020;369:m1401.
- NHS England (2020). A&E Attendances and Emergency Admissions 2020-21. Available at: https://www.england.nhs.uk/statistics/statistical-work-areas/ae-waiting-times-and-activity/ae-attendances-and-emergency-admissions-2020-21.
- Royal College of Surgeons England (2020). Clinical guide to surgical prioritisation during the coronavirus pandemic. Available at: https://www.rcseng.ac.uk/coronavirus/surgical-prioritisation-guidance.
- Ferguson NM, Laydon D, Nedjati-Gilani G, Imai N, Ainslie K, Baguelin M, et al. Impact of non-pharmaceutical interventions (NPIs) to reduce COVID-19 mortality and healthcare demand. Imperial College COVID-19 Response Team, London, March, 16. Available at: https://www.imperial.ac.uk/media/imperial-college/medicine/sph/ide/gida-fellowships/Imperial-College-COVID19-NPI-modelling-16-03-2020.pdf.
- NHS Health Education England (2020). COVID-19 and plans for management of medical and dental training programmes. Available at: https://www.hee.nhs.uk/sites/default/files/documents/COVID-19%20letter%20to%20Trusts%20and%20GP%20Practices%2010.03.2020.pdf.
- General Medical Council (2020). How we will continue to regulate in light of novel coronavirus (COVID-19). https://www.gmc-uk.org/news/news-archive/how-we-will-continue-to-regulate-in-light-of-novel-coronavirus.
- NHS Health Education England (2020). Supporting the COVID-19 response: Plans for Management of Medical Training Rotations. Available at: https://www.hee.nhs.uk/sites/default/files/documents/Plans%20for%20management%20of%20medical%20training%20rotations.pdf.
- Barking Havering & Redbridge University Hospitals (2020). Stakeholder update from Chief Executive Tony Chambers: 6 April 2020. Available at: https://www.bhrhospitals.nhs.uk/covid-19-bulletin/stakeholder-update-from-chief-executive-tony-chambers-6-april-2020-2329.
- Joint College of Surgical Trainees (2018). Certification Guidelines and Checklists. Available at: https://www.jcst.org/quality-assurance/certification-guidelines-and-checklists/.
- Burke J. The implications for surgical trainees in the delivery of care and training. RCS The Bulletin. 2020;102(S1):3.
- Hampton M, Clark M, Baxter I, Stevens R, Flatt E, Murray J, Wembridge K. The effects of a UK lockdown on orthopaedic trauma admissions and surgical cases. Bone Jt Open. 2020;1(5):137-143.
- Janbabi G, Razavi S, Dabbagh A. How to manage perioperative patient flow during COVID-19 pandemic: a narrative review. J Cell Mol Anesth. 2020;5(1):47-56.
- Barking, Havering and Redbridge University Hospitals NHS Trust (2020).
- Pareek M, Bangash MN, Pareek N, Pan D, Sze S, Minhas JS, et al. Ethnicity and COVID-19: an urgent public health research priority. Lancet. 2020;395(10234):1421-2.
- Lydall R (2020) London’s hospitals discharge thousands of virus patients. Evening Stand. Available at: https://www.standard.co.uk/news/health/8000-london-hospital-virus-patients-discharged-a4423136.html.
- British Orthopaedic Association (2020). Re-starting non-urgent trauma and orthopaedic care: Full guidance. Available at: https://www.boa.ac.uk/resources/boa-guidance-for-restart---full-doc---final2-pdf.html.
