The Indecision Grid
By Sunil Auplish
Consultant Orthopaedic Surgeon, York Hospitals NHS Trust
Corresponding author e-mail: [email protected]
Published 13th January 2022
Most of us have clear plans on how we would manage specific conditions. A fractured toe can usually be left alone, and a fractured neck of femur needs a surgical procedure.
However, there are many orthopaedic conditions for which both operative and non-operative treatments are viable options. This is especially true of orthopaedic trauma as demonstrated by randomised clinical trials for fractures of the proximal humerus (PRoFHER), distal radius (DRAFFT) and calcaneus (UK HeFT).
The decision of whether to operate for an injury is often made in fracture clinic, sometimes many days after the injury when partial union is present. The decision can be based as much on the health, lifestyle and attitudes of a patient as it is on the x-rays. These attributes vary hugely from patient to patient, and this adds to the complexity of decision making. Put simply - deciding what is best for a patient can sometimes be hard, and the prospect of making the wrong decision is always worrying.
The 'Indecision Grid' allows a clinician to evaluate the risks of operative and non-operative treatment, and then discuss these options with a patient to arrive at a reasonable decision that the patient would contribute to and support.
The grid is based on the answer to two questions:
- Does the patient need an operation? (Yes or No)
- Will the patient get an operation? (Yes or No)
The grid is therefore a 2x2 table that has four possible outcomes:
- The patient needs an operation and gets one (e.g. hip fracture).
- The patient does not need an operation and does not get one (e.g. toe fracture).
- The patient doesn’t need an operation but gets one anyway.
- The patient needs an operation but doesn’t get one.
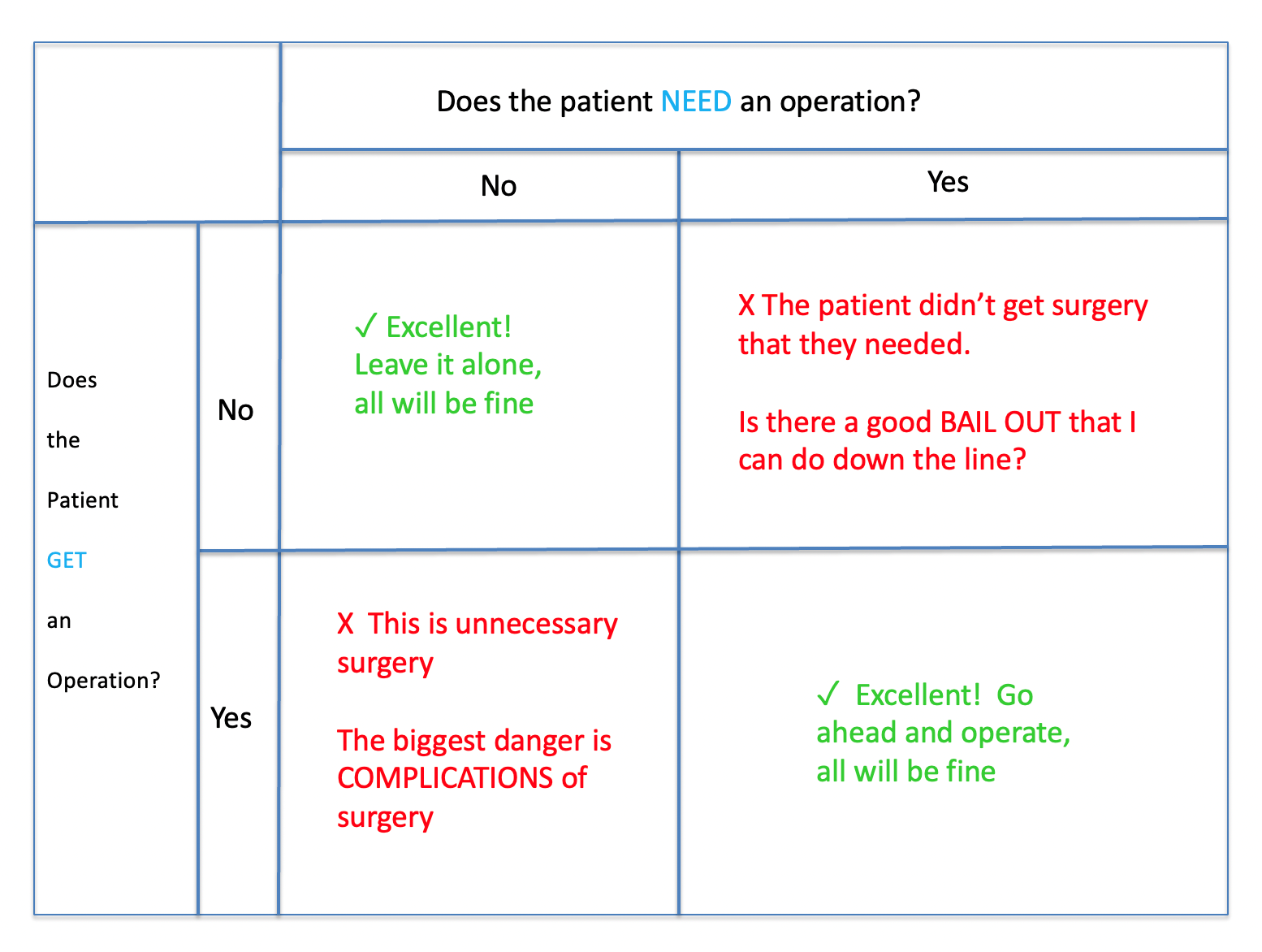
We don’t need to worry about patients in categories 1 and 2. Here, we know what to do and are confident that we are doing the right thing. We are concerned with patients in category 3 or 4 – which are the two categories where we will realise afterwards that the wrong decision has been made.
What is the problem with category 3? If the patient doesn’t need an operation but gets one anyway then they will have unnecessary surgery. They are likely to do well with surgery – think of a mildly displaced distal radius fracture that gets plated. The patient is out of plaster and using their hand quickly. The biggest danger for this group is therefore the risk of surgical complications. A bad infection would turn this great result into a disaster.
The patients in category 4 should have had surgery and didn’t get it. The biggest danger for this group is therefore poor outcome with non-operative treatment. The question that needs to be asked is “what is the bailout if they do badly without surgery?”. If there is a good procedure that can be done down the line to resolve the situation, then non-operative treatment is fine, but if there is no good bailout down the line then there is a stronger need to offer surgery at the time of injury.
The question of whether to operate is therefore one of comparing complication risks vs. the success of bailout surgery. Bailout/salvage surgery usually consists of osteotomy for bony deformity, and fusion or arthroplasty for joint disease, but there are specific procedures for different joints that are worth becoming familiar with.
Using a distal radius fracture as an example, if the patient is fit, healthy and sporty then we are less concerned about surgical risks than if they are frail, have lower functional demands and many co-morbidities in whom we are less likely to offer surgery.
The bailout for an extra-articular distal radius fracture malunion is an osteotomy, which has a good outcome as the joint surface itself is not damaged and the bony anatomy can be restored to its rightful place. Non-operative treatment for extra-articular fractures is therefore less concerning if the decision turns out to be wrong and surgery is required later.
However, a displaced intra-articular fracture which undergoes malunion will lead to wrist arthritis. The bailout here is likely to be a partial or full wrist fusion which at the very least will cause a stiffened joint. In cases of displaced intra-articular fractures, we are more likely to offer surgery at the time of fracture to preserve the joint and try to prevent the need of a fusion in the future.
However, if the patient is clear that they do not want an operation, and if the bailout of partial or total wrist fusion in the future is acceptable to the patient then we can confidently choose non-operative treatment. We have all seen terrible intra-articular distal radius fractures that have somehow resulted in good clinical outcomes!
I draw the grid out in clinic in those moments of uncertainty and indecision. I explain the complications and bailouts to the patient by writing them in their respective quadrants. Doing this, I am able to come to a decision with the patient that we both think is the right one for them individually and that I feel is reasonable medically. I give the grid to the patient to take away with them. And if we get the decision wrong, then the patient trusts me to either treat the complication that occurs or to do the bailout surgery myself because these are problems that we have anticipated together.
I hope that you have enjoyed reading this and find it to be as useful in your daily practice as I have.
