The impact of orthopaedic service cutback during COVID-19 pandemic on geriatric hip fracture management in a public hospital
By Chi Kin Lo and Yiu Chung Wong
Department of Orthopaedics and Traumatology, Yan Chai Hospital, Hong Kong
Corresponding author e-mail: [email protected]
Published 26th August 2020
Introduction
The coronavirus disease 2019 (COVID-19) outbreak, which was declared pandemic by the World Health Organisation on 11th March 2020, had posed a major challenge for orthopaedic service worldwide. Change to hospital service configuration was made to cope with the surge of COVID-19 patients. Operating department staffs were deployed to medical departments. Orthopaedic procedures were cutback to lessen the use of personal protective equipment (PPE). Turnover time between surgical cases was lengthened due to PPE procedures. As a result, orthopaedic operative productivity declined substantially1.
On the other hand, the incidence of geriatric hip fracture, which was well-known for its high mortality and morbidity, remained unaffected during the pandemic period2.
The aim of this study was to identify the impact of COVID-19 pandemic on the treatment and early outcome of geriatric hip fracture patients.
Methods
This was a retrospective cohort study conducted in a single Hospital Authority (HA) hospital. All patients aged over 65 admitted through the Accident and Emergency Department and received hip fracture operation in the strictest lockdown period between March 2020 and May 2020 were studied. Data collected from patients who received geriatric hip fracture operation from March 2019 to May 2019 was used as control. Hip fracture was defined as trochanteric fracture and neck of femur fracture. Periprosthetic femoral fracture and polytrauma patients were excluded. All patient identities were anonymised for analysis. The study was approved by the institutional research committee.
Demographic data, treatment and outcome data were retrieved retrospectively from the Clinical Management System of HA. Demographic data included age, sex and type of fracture. Type of operation and time from admission to surgery (TTS) were identified. Postoperative outcomes were assessed by postoperative complications, return to theatre, 30-day mortality and length of hospital stay (LOS). The COVID-19 status of the patient in the study period was also assessed. Continuous variables were presented as mean and compared using Student’s t-test. Categorical variables were presented as absolute number and compared using Chi-squared test. A P-value of ≤0.05 was considered statistically significant.
Results
A total of 98 patients were reviewed in this study. The number of geriatric hip patients operated in the pandemic period was 46 compared to 52 in 2019. There was no significant difference in patient demographics, type of operation, TTS, postoperative complications among the study and control group, (see Table 1). Details of postoperative complications were presented in figure 1. None of the studied patients required return to theatre or died within 30 days after operation. The mean LOS was 5.81 days shorter in the pandemic period (p=0.045), (see Table 2). None of our patients had a positive COVID-19 result.
|
|
Patients operated in 2019 |
Patients operated in 2020 |
P value |
|
Mean Age (years) |
83.88 |
84.32 |
0.774 |
|
Gender |
|
|
|
|
Male |
17 |
13 |
|
|
Female |
35 |
33 |
0.635 |
|
Type of fracture |
|
|
|
|
Trochanteric |
27 |
27 |
|
|
Neck of femur |
25 |
19 |
0.453 |
|
Type of operation |
|
|
|
|
Fracture fixation |
30 |
33 |
|
|
Arthroplasty |
22 |
13 |
0.148 |
|
TTS (days) |
3.23 |
3.83 |
0.362 |
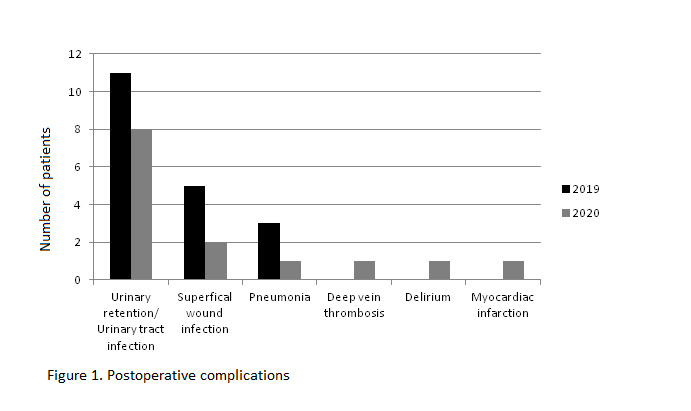
Figure 1: Postoperative complications
|
|
Patients operated in 2019 |
Patients operated in 2020 |
P value |
|
Postoperative complications |
19 |
14 |
0.523 |
|
Return to theatre |
0 |
0 |
|
|
30-day mortality |
0 |
0 |
|
|
LOS (days) |
35.83 |
30.02 |
0.045 |
Abbreviations: LOS = length of hospital stay
Discussion
Geriatric hip fracture accounted for substantial workload in orthopaedics departments; with more than 14,000 cases managed in Hong Kong each year3. Extensive studies had demonstrated the importance of early operation to reduce mortality and morbidity of geriatric hip fracture patients4-6. With the marked cutback of orthopaedic service during COVID-19 pandemic, studies demonstrated a delay in time to surgery and potential increased complications7-9. This study tried to identify the impact of COVID-19 on the treatment and early postoperative outcome of geriatric hip fracture patients.
In the strictest lockdown period between March and May 2020, our orthopaedic operative sessions were reduced by 60 percent, leaving only three whole-day sessions and a daily emergency operating list which was shared among general surgery, orthopaedic surgery and otolaryngology. Our department therefore decided to prioritise urgent cases while delaying elective operations by focusing our resources on three disease categories: (1) acute fracture, (2) musculoskeletal infection and (3) disease causing neurovascular compromise. Our study showed that we were able to maintain the standard of care for geriatric hip fracture by implementing measures to offset the detrimental effect of service disruption. There were no delay in surgery, no increased postoperative complications nor 30-day mortality compared to pre-pandemic period.
Our study found that the LOS as reduced by 5.81 days during the pandemic period, which aligned with overseas studies1, 7. In our institute, hip fracture patients were sent to the rehabilitation service within our hospital immediately after operation. The shortened LOS was explained by the effort made by our rehabilitation team to facilitate early discharge to avoid in-hospital transmission of COVID-19.
With the decline in incidence of COVID-19 by the end of May 2020, elective orthopaedic surgery was resumed gradually10. However, the condition of COVID-19 pandemic remained critical across the globe, we must therefore prepare for the surge of COVID-19 in the future. Our study looked into the impact of COVID-19 pandemic on geriatric fracture management and shared our experience to cope with the massive cutback of orthopaedic service. Health authority should formulate guidelines to prepare for service cutback and determine which procedure to be continued when the 'second wave' arrived11,12.
We acknowledge the retrospective nature of our study and that our analysis was highly dependent on the accuracy of documentation. Our results also reflected the clinical result of a single centre.
Conclusion
Our study showed that by prioritizing urgent orthopaedic cases while delaying elective operations, we were able to maintain the standard of care for geriatric hip fracture patients. Emphasis on expediting discharge resulted in shorted LOS in the COVID-19 pandemic.
References
1. Malik-Tabassum K, Crooks M, Robertson A, To C, Maling L, Selmon G. Management of hip fractures during the COVID-19 pandemic at a high-volume hip fracture unit in the United Kingdom. J Orthop. 2020;20:332-7.
2. Jain VK, Lal H, Patralekh MK, Vaishya R. Fracture management during COVID-19 pandemic: A systematic review and meta-analysis. J Clin Orthop Trauma. 2020;11(Suppl 4):S431-S41.
3. Leung KS, Yuen WF, Ngai WK, Lam CY, Lau TW, Lee KB, Cheung WH. How well are we managing fragility hip fractures? A narrative report on the review with the attempt to setup a Fragility Fracture Registry in Hong Kong. Hong Kong Med J. 2017;23(3):264-71.
4. Al-Ani AN, Samuelsson B, Tidermark J, Norling Å, Ekström W, Cederholm T, Hedström M. Early operation on patients with a hip fracture improved the ability to return to independent living: a prospective study of 850 patients. JBJS. 2008;90(7):1436-42.
5. Liu KK, Ho AWH, Wong SH. Early surgery for Hong Kong Chinese elderly patients with hip fracture reduces short-term and long-term mortality. Hong Kong Med J. 2017;23(4):374-80.
6. Klestil T, Röder C, Stotter C, Winkler B, Nehrer S, Lutz M, Nussbaumer-Streit B. Impact of timing of surgery in elderly hip fracture patients: a systematic review and meta-analysis. Scientific Reports. 2018;8(1):1-15.
7. Williams J, Ajeet Kumar. The effect of the COVID-19 pandemic on hip fracture care. The Transient Journal. April 2020. Available at: https://www.boa.ac.uk/resources/the-effect-of-the-covid-19-pandemic-on-hip-fracture-care.html.
8. Catellani F, Coscione A, D’Ambrosi R, Usai L, Roscitano C, Fiorentino G. Treatment of proximal femoral fragility fractures in patients with COVID-19 during the SARS-CoV-2 outbreak in northern Italy. J Bone Joint Surg Am. 2020;102(12):e58
9. Napoli N, Elderkin AL, Kiel DP, Khosla S. Managing fragility fractures during the COVID-19 pandemic. Nat Rev Endocrinol. 2020;16(9):467-8.
10. Iyengar KP, Jain VK, Vaish A, Vaishya R, Maini L, Lal H. Post COVID-19: Planning strategies to resume orthopaedic surgery–challenges and considerations. J Clin Orthop Trauma. 2020;11(Suppl 3):S291-S295.
11. Sarac NJ, Sarac BA, Schoenbrunner AR, Janis JE, Harrison RK, Phieffer LS, et al. A review of state guidelines for elective orthopaedic procedures during the COVID-19 outbreak. J Bone Joint Surg Am. 2020;102(11):942-5.
12. Liebensteiner MC, Khosravi I, Hirschmann MT, Heuberer PR. Massive cutback in orthopaedic healthcare services due to the COVID-19 pandemic. Knee Surg Sports Traumatol Arthrosc. 2020;28(6):1705-11.
