Is the combination of a femur fracture a COVID-19 in the over 65s as bad as we think?
A study of current inpatient mortality of these patients in the Trauma and Orthopaedic department at Queen Alexandra Hospital, Portsmouth, between 1st March and 17th May 2020
By Alex Witek and Phil Sauvé
Department of Trauma & Orthopaedics, Queen Alexandra Hospital, Portsmouth, UK
Corresponding author email: [email protected]
Published 04 June 2020
Summary point
Between 1st March and 17th May 2020 in our department the in-patient mortality for patients over 65, admitted with a femur fracture, who went on to test positive for COVID-19 as an inpatient was 42.9%, increasing to 55.6% when including those who tested negative, but due to high clinical suspicion, were treated as positive.
Abstract
The COVID-19 pandemic that has swept the world in the first five months of 2020 is like nothing encountered in recent times. It has sparked global cooperation and sharing of information on a scale not seen before, particularly within the medical community as each country the virus moves to learns new lessons to pass on to the next devastated nation. That being said, rumours can quickly become intertwined with fact, thus potentially skewing ideas and practice to the detriment of patient care. There are certain constants in hospital admissions in the United Kingdom (UK) each year, one such is the number of hip fractures, usually around 65,000 to 75,000. It is safe to assume, due to the patient group, that this number of admissions would continue relatively unaffected despite the pandemic and any measures imposed by a government to restrict movement of people.
This study set out to assess the inpatient mortality of patients over 65 who were admitted with a femur fracture who then went on to test positive for COVID-19 as an inpatient, and to provide a figure based on fact. The study was conducted looking at all such patients admitted between the 1st March 2020 and the 17th May 2020. The idea was to give a mortality percentage as things stood in the department as of 6am on 18th May.
The findings showed a mortality rate of 42.9% if a patient tested positive for COVID-19 after admission with a femur fracture. However, due to the limitations of the swab and PCR testing for COVID-19, those patients who were treated as positive due to a high clinical suspicion despite testing negative, were also included, producing a mortality rate of 55.6%. The Office for National Statistics (ONS) recently published data for April showing that nationally in those aged over 65 years the proportion of total deaths that were due to COVID-19 was between 34-40%, whilst our patient group showed a rate of 55.6%, as expected higher than in the general population at this age.
As this study is published in the middle of a pandemic there are limitations to what can be accurately deduced currently. For example, 45 of the patient group remain as inpatients at the time of writing and two deaths are awaiting a post mortem. This study also only used inpatient mortality as the majority of patients included have not reached 30 days post hip fracture in order to produce an accurate 30-day mortality rate.
This study does however, give scope to continue looking at this patient group as the pandemic evolves, and to then follow them up in due course and evaluate the true numbers. It achieves its aims of providing a current evaluation of mortality in this patient group mid pandemic, thus providing helpful information to healthcare professionals they otherwise wouldn’t receive until well after the event itself.
Introduction
As the COVID-19 pandemic began to spread in early 2020, very little was known about the disease, its origins and its consequences. Now, months down the line, and with a global sharing of knowledge the likes of which have never been seen before, we are beginning to learn more and more, helping to guide our care as healthcare professionals. That being said, a long list of unknowns remains, and now, as each medical specialty looks to begin elective work once again, the medical community as a whole needs to look at what affect this disease has had on the population, especially looking at those affected alongside other 'normal' presentations. In the case of orthopaedics one patient group that was always going to keep coming in were the elderly hip fractures. With 65,000-75,000 hip fractures admitted to UK hospitals each year1 equating to on average 5,400 - 6,250 a month, there was likely going to still be a regular influx of these patients during the pandemic. This patient group are elderly and frail, most often suffering innocuous falls at home, be it in their own residence or a residential or nursing home, and so a nationwide lockdown may well not decrease the number of admissions with hip fractures. The decision was made to include all femur fractures to bring it in line with recent thinking that all fragility femur fractures occur in generally the same population group, and as such all of them, not just hip fractures will be receiving their own best practice tariff in the next two years.
This study set out to provide a real time update to our trauma and orthopaedic department about how these patients are doing and the outcome following a femur fracture during this pandemic. The modern phenomenon of spreading misinformation via social media and online was further highlighted during this pandemic, with prominent world leaders even proposing new, unproven, treatments for COVID-19 and even commencing themselves as subjects of early clinical trials2. In a less prominent, widely distributed way, rumours spread within the medical profession regarding the outcomes and mortality of patients contracting COVID-19 alongside other medical problems, not backed up by any data or studies, but repeated to colleagues as fact.
The aim of this study is to look at the in-patient mortality of patients who sustain a femur fracture and test positive for COVID-19 during the same hospital stay during this pandemic. This write up has been completed mid pandemic in order to give colleagues an idea, based on current data from our department, of what this rate really is, and so give them the data to inform discussions with patients and their families, from the consent process for operative intervention to prognosis, as well as to help guide any difficult management decisions that may yet come up.
Method
The patient list was compiled from the departmental trauma database that documents all new admissions and new post-operative patients. Data is entered onto this Microsoft Access based database prospectively for each patient admitted under orthopaedics at QAH and is password protected. Patients were taken from the 1st March 2020 up to and including the 17th May 2020.
Patients were included in this study if they were over 65 years old and had one of – intracapsular neck of femur fracture, extracapsular neck of femur fracture, subtrochanteric femur fracture, shaft of femur fracture, distal femur fracture or periprosthetic femur fracture. From the department database the co-morbidities and operation date could also be documented. Each patient was then searched on the other hospital systems, (OCEANO and ICE primarily) to document the remaining data required – admission date, discharge date, COVID-19 swab requests, COVID-19 swab results and death certificate outcome, whilst also checking co-morbidities. The data compiled was then analysed looking at the raw numbers of positive COVID-19 cases and deaths within the group. Further in depth statistical analysis has not been done due to the nature of this study being ongoing, with patients still in hospital and some deaths still awaiting post mortems.
Results
Over the selected time period there were 163 patients admitted to QAH who satisfied the inclusion criteria. Of the 163 patients included, 24.5% were male and 75.5% were female. The anatomical fracture types were also documented to aid further analysis in the future. Over this period the majority of hip fractures admitted to QAH were intracapsular (n=100), with also a large number of extracapsular fractures, and then an even spread of more distal fractures. One patient was categorised as 'other' as the admission was due to a failure of a distal locking plate at the level of a non-union, (see Table 2).
| Male | Female | Total |
| 40 | 123 | 163 |
| Intracapsular | Extracapsular | Subtrochanteric | Shaft | Distal femur | Periprosthetic | Other |
| 100 | 41 | 6 | 3 | 7 | 5 | 1 |
The patient group was then broken down by the outcome of their COVID-19 test swab. As the weeks went on the testing of inpatients gradually increased, with 100% of patients admitted during May, at the point of this study, being swabbed on admission (See Figure 1). Of the 163 patients included in this study, 109 were tested during the inpatient stay, with 102 negative and seven positive results. Of these seven positive results, three patients died.
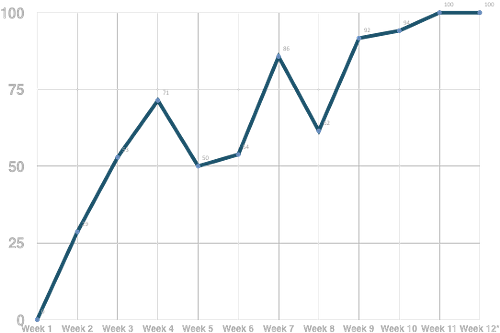
Figure 1: Percentage of admissions with a femur fracture, by week, tested for COVID-19 during admission
| Total patients | Tested for COVID-19 | Negative for COVID-19 | Positive for COVID-19 | Deaths with positive COVID-19 result |
| 163 | 109 | 102 | 7 | 3 |
| Total deaths | Never tested | Negative and NO clinical suspicion | Negative BUT high clinical suspicion | Positive for COVID-19 |
| 9 | 1 | 3 | 2 | 3 |
Of the nine deaths, four were intracapsular neck of femur fractures, two were extracapsular and then one each of distal femur, periprosthetic and subtrochanteric fractures, reasonably matching the spread of each fracture type in the group as a whole.
Each death was analysed to assess whether the COVID-19 positive deaths had a higher number of co-morbidities than the COVID-19 negative deaths, (see Table 5). The average number of co-morbidities for the COVID-19 negative deaths was 5.33, whilst the average for the COVID-19 positive deaths was 3. When including the negative but high clinical suspicion cases as positive deaths, the average number of co-morbidites is 2.8.
| Death | COVID-19 result | Co-morbidities | No. of co-morbidities |
| 1 | Not tested | AF, CCF, valvular heart disease, osteoporosis | 4 |
| 2 | Negative | AF, CKD, valvular heart disease | 3 |
| 3 | Negative | AF, CCF, T2DM, OSA, hypothyroid, osteoarthritis | 6 |
| 4 | Negative | CKD, HTN, IHD, PVD, Bladder cancer, valvular heart disease, previous TB - lobectomy | 7 |
| 5 | Negative BUT high suspicion | Dementia, hiatus hernia | 2 |
| 6 | Negative BUT high suspicion | COPD, HTN, IHD | 3 |
| 7 | Positive | Dementia, osteoarthritis | 2 |
| 8 | Positive | Chronic SDH, PVD | 2 |
| 9 | Positive | AF, CKD, CVD, T2DM, AAA | 5 |
From these overall numbers it was calculated that the in hospital mortality if a patient has a femur fracture as well as a positive swab result was 42.9%. If the high clinical suspicion but negative swab result patients are also included as positive COVID-19, the mortality is 55.6%. This was calculated due to there being seven positive results, with three resultant deaths. To include those treated as positive due to high clinical suspicion then adds in two more ‘positive’ results and deaths, hence five deaths out of nine (7+2) ‘positive’ patients. As a proportion of total deaths there were nine deaths of which five were positive or negative with high clinical suspicion, therefore 55.6% of all deaths were due to COVID-19 as things stand. Two post mortems are awaited and this value may change.
To provide context to the study so far, the National Hip Fracture Database was interrogated to get previous years data3. The NHFD uses 30-day mortality and so the comparison is not like-for-like, however our crude mortality as inpatients for this period currently sits at 4.8% (only comparing hip fractures), in comparison to 3.1% to 3.8% 30-day mortality for hip fractures at QAH for the same time last year, (see Table 6).
| March 2017 | June 2017 | March 2018 | June 2018 | March 2019 | June 2019 | COVID-19 period 2020 | |
| Crude mortality (annualised) | 4.3% | 5.3% | 4.7% | 3.8% | 3.8% | 3.1% | |
| Crude mortality as inpatient | 4.8% |
Discussion and conclusion
This study set out to provide data from a relatively high volume hip fracture unit regarding femur fractures, COVID-19 and the associated mortality as inpatients during the COVID-19 pandemic. When including the negative, but high clinical suspicion patients, the mortality for this patient group sits at 55.6% as an inpatient. It is reasonable to include the ‘negative but high clinical suspicion’ deaths as the swab and PCR test used to detect COVID-19 has been criticised, and often quoted as having a sensitivity of around 60-70% with a larger Chinese study giving a range from 53-89%4,5, however this figure is still up for debate due to the number of variables in terms of swab location (nasopharynx vs oropharynx), technique, days after illness onset swab performed and reagent used5.
All of the positive swab results were recorded after admission, with four positive results coming post-operatively and three pre-operatively. Of those three that went to theatre as known positive for COVID-19, two have been discharged home and the third remains as an inpatient. It would be reasonable to assume that the strain of a major orthopaedic operation could be too much for those patients going to theatre with both COVID-19 and a recent femur fracture, however these numbers, whilst limited currently, would go against that. It seems the order of events may not be key, more the severity of their COVID-19 infection and their pre-existing physiological reserve.
Out of the positive and negative with high clinical suspicion deaths, none were swabbed in the Emergency Department. Four had no symptoms there and so this was reasonable, one however did have a raised temperature in the Emergency Department however wasn’t swabbed, this patient was later swabbed when having raised temperatures two days post-op and subsequently tested positive for COVID-19. This patient potentially had COVID-19 on admission, however they were admitted in early March when the differential diagnosis was not so at the forefront of peoples minds.
To have only seven patients positive for COVID-19 over this period gives some indication at the success of the hospital policies brought in early on. The department quickly split into ‘dirty’ and ‘clean’ wards, and patients kept apart whilst awaiting swab results. PPE protocols brought in seem to have helped reduce transmission between patients and staff, however we will only have a proper idea of this looking back a few months down the line and including more of the hospital for greater numbers.
What can be deduced from this study to date is that, unfortunately for this patient population, if they are admitted to hospital due to a hip or femur fracture and subsequently go on to test positive for COVID-19 or develop symptoms consistent with COVID-19, then there is a greater than 50% chance that they will not survive that admission.
To provide context, the Office for National Statistics have released the report for April 2020 regarding overall mortality, which showed that the percentage of overall deaths due to COVID-19 in England for 65-74 year olds in April was 39%, for 75-84 year olds 40.1% and over 85s, 34%6. This is a percentage of the total deaths for that age group demonstrating, for example, that 40% of all deaths in April 2020 for persons aged 75-84 were due to COVID-19. The mortality rate as a total of all deaths in this patient group of over 65 year olds in this study was found to be 55.6%, and is therefore higher than would otherwise be expected in these age groups.
The idea of this study as outlined above was to give some real time data and analysis of what is happening with these patients in the middle of this global pandemic. This report will hopefully give other medical professionals some basic information to help back up conversations that will be had with these patients and their families in the coming weeks and months from the consent process through to outcomes and prognosis, as well as to help guide decision making regarding those patients who potentially deteriorate during their hospital admission.
Limitations
This study can, and will, be expanded upon with time when it will be possible to firstly follow the remaining inpatients through their admission, whilst also continuing to build a larger patient group to analyse overall. There are still 45 out of the 163 patients in hospital awaiting discharge, included in the data above. Two of the deaths are awaiting a post mortem at the time of writing and so further detail may come of that which would need to be added. In the coming months, as patients reach 30 days post fracture and post-op, it would be possible to look at the 30-day mortality of this patient group and thus be able to compare them to previous years like-for-like. The mortality figures quoted here are as inpatients as that is our only measurable time frame currently.
References
- NICE (2017). Hip fracture management. Clinical Guideline [CG124]. Available at: https://www.nice.org.uk/guidance/cg124.
- BBC News. Coronavirus: Trump says he is taking unproven drug hydroxychloroquine. 19th May 2020. Available at: https://www.bbc.co.uk/news/world-us-canada-52717161.
- Royal College of Physicians (2020). National Hip Fracture Database. Available at: https://www.nhfd.co.uk/.
- Yang Y, Yang M, Shen C, Wang F, Yuan J, Liet J al. Evaluating the accuracy of different respiratory specimens in the laboratory diagnosis and monitoring the viral shedding of 2019-nCoV infections. medRxiv. 2020;2(11):20021493.
- Carver C, Jones N. Comparative accuracy of oropharyngeal and nasopharyngeal swabs for diagnosis of COVID-19. March 26th 2020, Centre for evidence based medicine: University of Oxford. Available at: https://www.cebm.net/covid-19/comparative-accuracy-of-oropharyngeal-and-nasopharyngeal-swabs-for-diagnosis-of-covid-19/.
- Office for National Statistics - ONS (2020). Deaths involving COVID-19, England and Wales: deaths occurring in April 2020. May 15th 2020. Available at: https://www.ons.gov.uk/releases/deathsinvolvingcovid19englandandwalesdeathsoccurringinapril2020.
