How can we make Trauma and Orthopaedics in the UK more Eco-friendly?
By Karolina WieczorekThird year medical student, Barts and The London School of Medicine and Dentistry
|
This essay was one of the runners-up in the 2022 BOA Medical Student Essay Prize How can we make Trauma & Orthopaedics in the UK more Eco-friendly? |
Introduction
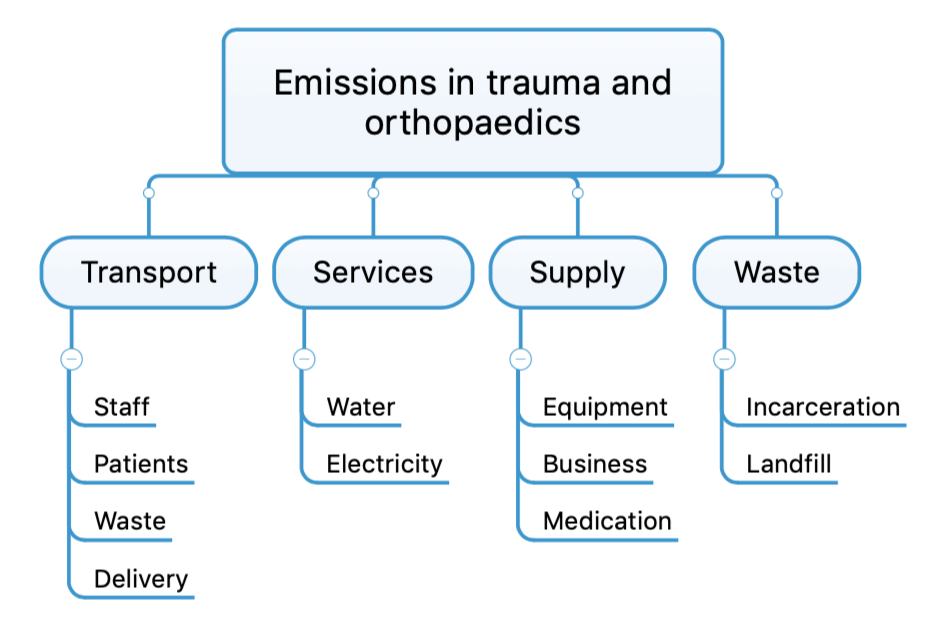
Sustainability is a concept of growing importance in modern healthcare. It includes introducing ecologically friendly solutions to preserve natural balance in resources for future generations1. NHS England is dedicated to meeting these aims by fulfilling the UN Sustainable Development Goals and introducing a net-zero carbon emission from 20402. Currently, over 27 million tons of carbon emissions come from the healthcare system, which constitutes 4% of the total, national emissions3. Trauma and Orthopaedics contribute to emissions more significantly than other specialties, and therefore pose as the perfect candidate specialties to be incentivised to pursue 'lean healthcare' initiatives to ensure environmental stability by reducing emissions outlined in Figure 14.
The number of orthopaedic surgeries is predicted to increase within a rapidly aging population and may soon surpass other specialities with regards to the total annual number of procedures performed5. A review by Rizan et al. identified that the highest emissions of greenhouse gases in surgery stem from electricity use in theatres, non-reusable equipment and aesthetic gases6. As outlined in Table 1, a total knee arthroplasty produces, on average, up to 13.3 kg of surgical waste6. At a larger scale, a trauma centre in USA estimated that in a year carbon dioxide emissions were equal to driving up to 196 cars for a year7.
|
Type of surgery |
Waste produced |
|
Primary hip arthroplasty |
5.2 kg noncontaminated waste8 up to 14 kg9 |
|
Total hip arthroplasty |
12 kg, 5.8 kg recyclable8 |
|
Total knee replacement |
11.6 kg9 to 13.4 kg10 |
|
Facet joint injection |
1.8 kg9 |
|
Shoulder arthroplasty |
0.55 % of all implants to go waste11 |
Table 1. Review of literature regarding the amount of waste produced in different
types of surgical procedures.
These significant emissions can be reduced though the introducing of innovative solutions, inspired by the tried-and-true three R’s principle: reuse, reduce, recycle12.
Reduce
Surgery often employs the use of large numbers of 'overage' items, which are prepared but not actively used. This not only adds financial costs but also increases the emissions of the precedures13. A simple solution to reduce the amounts of waste is redesigning the surgical trays and packs using ‘lean’ optimisation14. Less equipment has not only decreased the number of tools on trays and the cost of their preparation by half but also lowered turnover times of the operating rooms by almost an hour15. The same model could be applied to medication, to prepare drugs using a 'just-in-time' strategy rather than 'in case of emergency'.
Another factor majorly contributing to emissions in trauma and orthopaedics are anaesthetics gases, responsible for up to 42% of the emitted carbon dioxide. A solution to this would be incentives to decrease aesthetic gas use and choosing low global warming potential (GWP) options, such as switching from desflurane to intravenous anesthesia16. Other strategies include gas capture systems and low gas ventilators to decrease the flow during maintenance of anesthesia17.
Energy use constitutes the next highest source of emissions in orthopaedic surgery, with 25% of hospital operating costs spent towards meeting energy needs. In the span of a year, a surgical theatre is estimated to consume as much energy during as over 200 houses18, which given that they are unoccupied 25% of the time, justifies the urgent need for reducing unnecessary energy use. Examples of targeted solutions are outlined in Table 2.
|
Strategies to reduce energy use in surgery19 |
|
Adjusting thermostats, using double glazed window, high quality insulation |
|
LED or low-mercury bulbs, motion sensors, manual light switching |
|
Solar panels and other renewable energy sources |
|
Divest from carbon emission-rich energy providers |
|
Switching off computers and other equipment not in use |
|
Power and heat units combined |
|
Energy-efficient medical and nonmedical equipment |
|
Smart hospital infrastructure and OR design |
Table 2. Strategies to reduce use in energy in orthopaedics and trauma.
Reuse
Another important strategy in surgery, which has been demonstrated to have the potential to reduce emissions is reusing various pieces of equipment, such as external fixators. Doctors and patients are often sceptical about re-using surgical tools, however a randomised control trial showed no increase in infections rates after replacing and sterilising key parts of the device20. Waste can also be reduced by donating unused materials to schools or hospitals to divert them from landfills and decrease disposal-related emissions such as transportation. Innovative solutions outside of surgery include replacing single-use materials with innovative products such as Woodcast™, lightweight biodegradable material made from wood developed for use instead of plaster casts21. This pre-made cast visible in Figure 2, is free of toxins, quicker to fix in place without the need for water, sink, ventilation or any special equipment while saving an average hospital 500kg of waste per year22.

Figure 2: Woodcast OneStep – a pre-cut splint for ankle and wrist stabilisation.
Recycle
A different major factor contribution to carbon emissions in orthopaedic surgery is incorrect waste segregation. If waste was correctly separated and only clinical waste incarnated, up to half a billion pounds would be saved by the NHS per year and emissions would be cut by 75%.
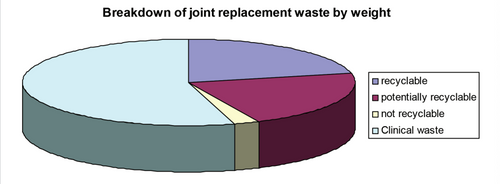
Figure 3 shows that a significant part of waste is recyclable, however as much as 90% of clinical waste is incorrect disposed of. Even though hazardous and medical waste represent a small portion of waste production, the costs of their disposal are significantly higher. A simple measure such as making non-hazardous waste bags more available during surgery should encourage more careful waste segregation. Innovative technology such as Demolizer® can be used to melt sharp waste into non-hazardous waste for safe disposal23.
Many of the strategies rely on ongoing auditing, therefore data recording is a key step to monitoring progress. Certain barriers have been identified which stop people from implementing green solutions, those include: lack of leadership, lack of data and research, perceived infection risks, increased workload and resistance to change18. That is why teaching about environmental stewardship and circular economy in medical schools is important to ensure future environmental security, especially in specialties producing high emissions.
Conclusions
Trauma and orthopaedics significantly contribute to carbon emissions, however by introducing innovative solutions aiming to reuse, reduce and recycle waste, it is possible to reach the zero emissions goals set by the NHS. Numerous strategies employed on a small scale can have a major cumulative effect when efforts are combined to offset the environmental consequences of surgery’s life-saving endeavours.
References
- Kuhlman T, Farrington J. What is Sustainability? Sustain Sci Pract Policy. 2010;2(11):3436-48.
- NHS England. Greener NHS. Available from: www.england.nhs.uk/greenernhs/a-net-zero-nhs/areas-of-focus. [Accessed December 11, 2021].
- NHS England. Greener NHS. Delivering a ‘Net Zero’ National Health Service. Available from: www.england.nhs.uk/greenernhs/wp-content/uploads/sites/51/2020/10/delivering-a-net-zero-national-health-service.pdf.
- Zywiel MG, Delanois RE, McGrath MS, Ulrich SD, Duncan JL, Mont MA. Intraoperative waste of trauma implants: a cost burden to hospitals worth addressing? J Orthop Trauma. 2009;23(10):710-5.
- Royal College of Surgeons of England. Surgery and the NHS in numbers. Available from: www.rcseng.ac.uk/news-and-events/media-centre/media-background-briefings-and-statistics/surgery-and-the-nhs-in-numbers. [Accessed January 30, 2022].
- Rizan C, Steinbach I, Nicholson R, Lillywhite R, Reed M, Bhutta MF. The Carbon Footprint of Surgical Operations: A Systematic Review. Ann Surg. 2020;272(6):986-95.
- Kwakye G, Brat GA, Makary MA. Green surgical practices for health care. Arch Surg. 2011;146(2):131-6.
- Pavlou P, Gardiner J, Pili D, Tayton E. The environmental impact of large joint arthroplasty. Orthopaedic Proceedings. 2010;92-B(SUPP_IV):498.
- Southorn T, Norrish AR, Gardner K, Baxandall R. Reducing the carbon footprint of the operating theatre: a multicentre quality improvement report. J Perioper Pract. 2013;23(6):144-6.
- Lee RJ, Mears SC. Reducing and recycling in joint arthroplasty. J Arthroplasty. 2012;27(10):1757-60.
- Pfefferle KJ, Dilisio MF, Patti B, Fening SD, Junko JT. Transparency to Reduce Surgical Implant Waste. Clin Orthop Surg. 2015;7(2):207-10.
- 3Rs - Reduce, Reuse & Recycle - SustainableSA.com. Published 30 June 2012. Available from: www.sustainablesanantonio.com/practices-technology/reduce-reuse-recycle. [Accessed December 22, 2021].
- Thiel CL, Fiorin Carvalho R, Hess L, et al. Minimal Custom Pack Design and Wide-Awake Hand Surgery: Reducing Waste and Spending in the Orthopedic Operating Room. Hand. 2019;14(2):271-6.
- Cichos KH, Hyde ZB, Mabry SE, et al. Optimization of Orthopedic Surgical Instrument Trays: Lean Principles to Reduce Fixed Operating Room Expenses. J Arthroplasty. 2019;34(12):2834-40.
- Kellish AS, Shahi A, Tornsberg H, Miller L. What Is Orthopaedic Surgery’s Environmental Impact? Published online 4 April 2021. [Accessed January 29, 2022.]
- Whiting A, Tennison I, Roschnik S, Collins M. Surgery and the NHS carbon footprint. Bull R Coll Surg Engl. 2020;102(5):182-5.
- Liu L, McGain F, Kentish SE. Recovery of Sevoflurane Anesthetic Gas Using an Organosilica Membrane in Conjunction with a Scavenging System. Environ Sci Technol. 2021;55(5):3362-7.
- Wyssusek KH, Keys MT, van Zundert AAJ. Operating room greening initiatives - the old, the new, and the way forward: A narrative review. Waste Manag Res. 2019;37(1):3-19.
- Potera C. Strategies for greener hospital operating rooms. Environ Health Perspect. 2012;120(8):a306-7.
- Sung JK, Levin R, Siegel J, Einhorn TA, Creevy WR, Tornetta P 3rd. Reuse of external fixation components: a randomized trial. J Orthop Trauma. 2008;22(2):126-30; discussion 130-1.
- Industrial News Service. Eco-friendly splints developed for hospitals make their debut in sports. Available from: www.ins-news.com/en/100/1002/2758/Eco-friendly-splints-developed-for-hospitals-make-their-debut-in-sports.htm. [Accessed January 30, 2022].
- Woodcast. Available from: www.woodcast.com. [Accessed February 10, 2022].
- Gareth Chan, Lucy Sinclair, Chantelle Rizan, Stephen Bendall, Mahmood F Bhutta and Benedict Rogers. Sustainable orthopaedic surgery, An oxymoron? Orthopaedics Online. Available from: www.boa.ac.uk/resources/knowledge-hub/sustainable-orthopaedic-surgery-an-oxymoron.html. [Accessed January 28, 2022].
