Hand and wrist fractures: The ‘SBCDS’ approach
By Liam Donnelly, Matthew Pritchard, Natalie Tao and Phil Storey
St Mary's Hospital - Imperial College Healthcare NHS Trust
Corresponding author e-mail: [email protected]
Published 28 October 2021
Introduction
The hand is one of the most important functional parts of the human body and is needed for many daily activities. Injuries of the hand and wrist are frequently encountered in the emergency department, accounting for 20% of acute fractures1. The goal of treatment is rapid restoration of function. Hand injuries that are missed or inappropriately diagnosed may result in severe long-term functional disability.
The first point of contact in the emergency department is usually a junior doctor, or possibly a medical student on clinical placement. In the management of hand injuries clinical examination and plain radiographs are the main diagnostic tools. Therefore, the ability to interpret plain radiographs and diagnose hand fractures is an important skill for emergency department doctors, particularly junior doctors who may be less confident doing so.
This report proposes ‘SBCDS’ (Skin, Bone, Configuration, Displacement, Stability), a systematic approach to interpreting hand and wrist plain radiographs. This approach aims to assist junior doctors with the interpretation and communication of hand and wrist plain radiographs when referring to the orthopaedic team, in a simple and effective manner.
Hand fracture aetiology
A hand fracture may involve a break of one or multiple metacarpal bones and/or the phalanges, the small bones of the digits. The most common bones to be fractured are those of the little finger2. Certain patterns of fracture arise from different mechanisms of injury. These include direct contact, crushing, twisting and falling. The mechanisms of injury vary between age groups, with younger people predominantly experiencing fractures in contact sport, middle aged people in work-related activities and the elderly through falls. Additionally, men are about 1.5 times more likely to experience a hand fracture than women.
The ‘SBCDS’ approach
The ‘SBCDS’ approach provides a systematic way of interpreting and describing hand and wrist plain radiographs. A detailed history of the mechanism of injury and clinical examination correlated with radiographic findings should enable an accurate diagnosis of hand and wrist fractures. Clinical examination is essential to determine the appropriate radiographic views and to direct radiographic evaluation for subtle injuries. As a general rule, at least two different views that are in planes that are 90 degrees to each other are required for accurate radiographic evaluation.
In the context of an injury, forces pass through soft tissue (skin, nerve, vessel, tendon and ligament) to bone. As soft tissue injuries are not readily seen on plain radiographs, they will not be addressed in detail in the ‘SBCDS’ approach. However, it is vital to consider soft tissue injury in relation to the mechanism of injury; failure to detect them could lead to complications such as tendon rupture or joint infection.
Not all the descriptive terms included in the approach are required for every fracture. However, having a systematic approach such as ‘SBCDS’ will ensure that all relevant details are considered, and a clear structure for interpreting and communicating radiographs will be followed. Imagine you are describing the radiograph over the phone!
The ‘SBCDS’ approach outline
- Skin
- Determine whether it is an open (compound) or closed fracture.
- Bone
- Identify bone(s) and part of bone(s) fractured.
- Establish if fracture is intra- or extra-articular.
- Configuration
- Is the bone fractured into two fragments (simple) or more than two fragments (comminuted)?
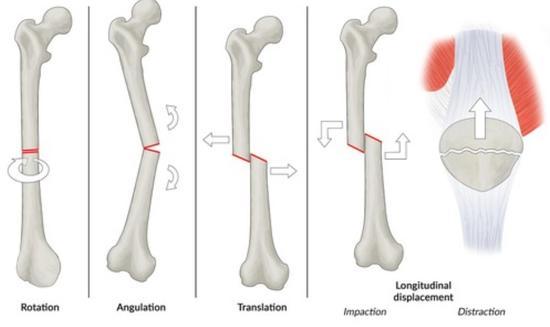
- Determine fracture type: transverse, oblique or spiral (see Figure 1).
![shutterstock_121363498 [Converted].jpg](https://www.boa.ac.uk/static/298c1009-457d-4c0d-800fba2d19dfde69/550x385_highestperformance__4a7c7e45a350/shutterstock121363498-Converted.jpg)
Figure 1
- Displacement
- Assess the degree of displacement to determine the need for reduction.
- Consider: angulation (°), translation (%), rotation (°) and shortening (mm). (Figure 2).
- Stability
- Joint instability is present when a joint has greater than normal movement in any plane3. Physical examination is required to determine if fractures are stable or unstable.
- Unstable joints are likely to displace if not immobilised (either using surgical fixation or non-surgical methods such as braces, splints or casts). Stable fractures are unlikely to displace and often require protection or activity modification.
Examples Using The ‘SBCDS’ Approach
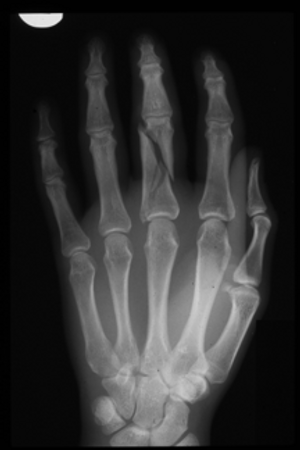
Example 1 - Metacarpal bones
- Skin
- Closed (known from examination).
- Bone
- Diaphysis (shaft).
- Right fourth (ring finger) metacarpal.
- Configuration
- Simple (two fragments).
- Transverse.
- Displacement*
- 50% translation.
- 20° angulation (also need lateral X-ray to determine this).
- 2mm of shortening.
- Examination of the finger in flexion showed no rotational malalignment or extensor lag.
- Stability
- A transverse fracture if ‘hitched’ and protected (either by use of a cast or splint or by activity modification) may not move into an unacceptable position.

*Note: The acceptability of the degree of displacement and the likelihood of stability requires discussion with the patient. This is a clinical judgment and often experts will disagree.
This should be reported as:
‘A closed fracture of the diaphysis of the right fourth metacarpal. It is a simple, transverse fracture with 50% translation and 20 degrees of angulation.’
Example 2 - Metacarpal bones
- Skin
- Closed.
- Bone
- Neck of fifth (little finger) metacarpal.
- Configuration
- Comminuted.
- Transverse.
- Displacement
- 30° volar (palmar) angulation (apex dorsal).
- Clinical examination reveals no rotation on flexion and 20 degrees of extensor lag.
- Stability
- Stable - impacted fractures are typically quite stable.

This should be reported as:
‘A closed fracture of the neck of the fiftth metacarpal bone. It is a comminuted, transverse fracture with 30 degrees of volar angulation.’
(This injury is also known as ‘boxer’s fracture’ and has a predictable mechanism of injury following punching solid objects. It requires urgent referral to a hand surgeon for a joint washout if it is open.)
Example 3 - Proximal phalanges
- Skin
- Closed.
- Bone
- Diaphysis (shaft).
- Proximal phalanx of middle finger.
- Intra-articular: just extends into metacarpophalangeal joint (MCPJ).
- Configuration
- Comminuted spiral fracture.
- Displacement
- Shortened and translated.
- Distal and proximal joints line up, and nails in normal orientation, so may not be rotated. Too painful to examine in flexion.
- Stability
- Unstable - comminuted fractures often unstable due to fragmentation of the bone into several pieces.
This should be reported as:
‘A closed comminuted spiral fracture of the diaphysis of the proximal phalanx of the middle finger. It is intra-articular, extending into the metacarpophalangeal joint, and is shortened and translated.’
Example 4 - Proximal phalanges
- Skin
- Closed.
- Bone
- Through metaphysis (Salter Harris 2) of the base of the ring finger proximal phalanx.
- Configuration
- Simple transverse.
- Displacement
- 20° ulnar angulation therefore needs reduction.
- Stability
- Stable.

This should be reported as:
‘A fracture at the base of the proximal phalanx of the fourth finger through the metaphysis. It is a simple transverse fracture with 20 degrees of ulnar angulation.’
Example 5 - Carpal fracture
- Skin
- Closed.
- Bone
- Trapezium.
- Extends intra-articularly into carpometacarpal joint (CMCJ).
- Configuration
- Simple fracture.
- Displacement
- Minimally displaced.
- Stability
- Stable.

This should be reported as:
‘A closed fracture of the trapezium which extends into the carpometacarpal joint. It is a simple, minimally displaced fracture.’
Conclusion
The ‘SBCDS’ approach to interpreting and reporting hand and wrist radiographs can improve the method by which fractures are described. It is simple and systemic, making it an easy aide-memoire to employ at all levels of experience, including medical students.
References
- Coyle J, Naraghi A, Chan O. Hand and Wrist. BMJ. 2014 Mar 17;348:bmj.g2174.
- Van Onselen E, Karim R, Hage J, Ritt M. Prevalence and Distribution of Hand Fractures. J Hand Surg Br. 2003 Oct;28(5):491-5.
- Firestein G, Budd R, Gabriel S, Koretzky G, McInnes I, O'Dell J. Firestein & Kelley's textbook of rheumatology.
