Greener orthopaedics – Sustainability by saving the substance of life: Water
Jehan Zaib
Trauma and Orthopaedic Consultant, Hywel Dda UHB, West Wales
While Earth's surface is 70% water, water is not as limitless as it may seem. Nepal, despite holding 2.7% of the world’s freshwater, struggles with pollution and inadequate infrastructure, particularly in Kathmandu1. Similarly, the Netherlands faced water shortages after a 2018 heatwave2, while Egypt, dependent on the Nile for 97% of its water, is combating dwindling supplies due to population growth and upstream demands3. Even Tokyo, with ample rainfall, experiences periodic droughts4. The UK, projected to become warmer and drier by 2050, is already facing issues such as water waste due to aging infrastructure. These cases highlight the global nature of water scarcity, worsened by climate change, which affects regions in diverse ways and necessitates more efficient water management and conservation strategies5,6.
In 2002/2003, the NHS in England used 40.3 million cubic metres of water and produced 34.4 million cubic metres of sewage, leading to high financial and environmental costs. By implementing simple water-efficiency measures, the NHS could save up to 20% of its water costs, which equates to £9.5 million annually. These savings could be achieved with minimal investment through small infrastructure repairs and changes in staff behaviour. Some improvements may require initial funding but offer a quick return on investment. The Health Technical Memorandum emphasises the importance of efficient water management, considering the economic, environmental, and health-related benefits, while pointing out that taps alone waste 13% of water—around 400 litres a day—highlighting the urgent need for better efficiency7,8.
One of the ways water is wasted in trauma and orthopaedic operating theatres is by washing hands before surgery. Hand washing or surgical scrubbing before surgery has been a vital practice since the time of Lister, rooted in tradition and hygiene9. Historically, the duration of this procedure has significantly decreased, from 10 minutes in 1894 to five minutes by 19509. According to a 2008 WHO report, using alcohol rubs for bacterial clearance is just as effective as traditional surgical scrubs, achieving the same results in merely three minutes. The WHO and NICE guidelines recommend that the operating team should wash their hands prior to the first operation on the list using an aqueous antiseptic surgical solution, with a single-use brush or pick for the nails, and ensure that hands and nails are visibly clean. Before subsequent operations, hands should be washed using either an alcoholic hand rub or an antiseptic surgical solution. If hands are soiled, they should be washed again with an antiseptic surgical solution10. Notably, a five-minute hand washing session can waste up to 30 litres of water11, underscoring the importance of adopting more water-efficient practices such as alcohol rubs in medical settings. A study comparing different handwashing methods in the orthopaedic theatres found that an alcohol-only scrub reduced water usage by 85.5% compared to standard scrubbing, 64% compared to scrub nurse-assisted scrubbing, and 58% compared to self-washing, saving up to 1.9L per scrub12. Another study shows that switching to an alcohol-based hand rub for subsequent scrubs could save up to 82.29L per day for a major trauma list and 288.7L per day for a carpal tunnel release list13.
To further investigate this, we conducted a simple audit in our hospital on elective arthroplasty lists to assess the impact of different scrubbing methods on overall water usage by the surgical team. Observing three consecutive arthroplasty lists over a week, we recorded water usage during scrubbing by the operating and anaesthetic teams, with all members blinded to the study. The main challenge was calculating the water used due to sensor taps (Figure 1) delivering varying amounts of water per swipe. To address this, we collected water with a single swipe from each tap into a labelled drinking bottle (Figure 2) to measure the specific amount of water delivered. We noted that each tap dispensed different amounts of water per swipe. A third observer was tasked with counting the number of times the sensors were swiped for each scrub by individuals involved in surgery and then calculating the total water usage.

Figure 1: Water sensors

Figure 2: Labelled water bottle
The study included the anaesthetist, orthopaedic consultant surgeon, orthopaedic registrar, orthopaedic SHO, and scrub nurse. The senior surgeon adhered to a traditional approach, starting with a morning pre-scrub and using an alcohol rub for each case, except when hands were soiled. Over 14 lower limb primary arthroplasty cases, the team used a cumulative 193 litres of water, averaging 13.8 litres per case. This translated to 64 litres of water per scrub list, 38.6 litres per person per day, and 13.7 litres per arthroplasty. Notably, 59.5% (79 litres) of water consumption could have been saved just on hand scrubs by using standard guidelines. The anaesthetist, using alcohol rub for half the observed time, demonstrated the most conservative water usage, averaging 0.84 litres per case. The senior surgeon who followed the NICE guidelines averaged 1.1 litres per case, while the SHO and registrar following the traditional surgical scrub with water every time had the highest water consumption at 5.7 litres per case. The nurses collectively used 44.8 litres (Figure 3).
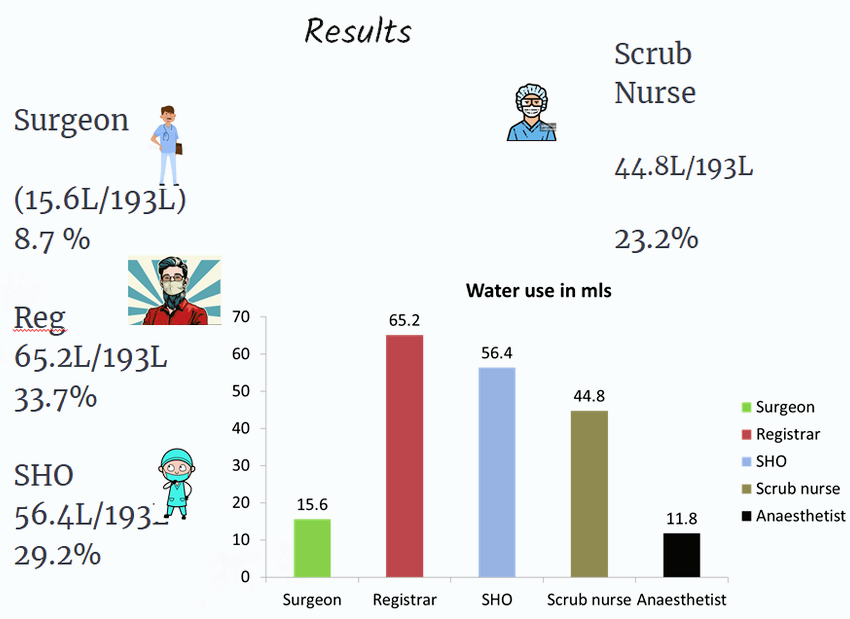
Figure 3: Study results
Our findings suggest that universally adopting alcohol rub, as endorsed by the WHO, can result in a 10-fold reduction in water usage, aligning with global health guidelines and highlighting the substantial potential for resource conservation in surgical procedures. The impact of following such a small guideline is significant financially and environmentally, with the potential to save 4,606 litres of water annually just on hand scrubs, reducing total water usage from 10,840 litres per year to 6,234 litres per year based on our observations.
Efficient water management is hampered by a lack of staff awareness, leading to potential savings in water bills and increased environmental integrity being overlooked in the past. The development of a water strategy should be seen as an opportunity to raise staff awareness as well as to gather input. Water use is an emotive issue, and staff should be informed of the project to develop a water strategy and be given regular updates during the process.
By making small changes, such as adopting alcohol rubs for hand hygiene as endorsed by the NICE guidelines, healthcare facilities can significantly reduce water usage. Our study has shown that such practices could save up to 59.5% of water consumption just on hand scrubs. Implementing these changes will not only conserve water but also contribute to climate-change mitigation by reducing the carbon footprint associated with water supply and treatment.
In conclusion, a comprehensive and inclusive water strategy is essential for the sustainable management of water resources in healthcare settings. It should prioritise staff engagement and education, identify and address patterns of water use, and implement evidence-based practices to achieve substantial water savings and environmental benefits.
References
-
Poudel N, Shaw R. Challenges of Urban Water Security and Drivers of Water Scarcity in Kathmandu Valley, Nepal. Urb Science. 2025;9(3):54.
- Flander Environment Agency (2018). Drought Management Plan. Retrieved from https://en.vmm.be.
- Elbasiouny H, Elbehiry F. (2020). Rice Production in Egypt: The Challenges of Climate Change and Water Deficiency. In: Ewis Omran, ES., Negm, A. (eds) Climate Change Impacts on Agriculture and Food Security in Egypt. Springer Water. Springer, Cham.
- Tokyo Metropolitan Government (2019). Tokyo's water supply system. Retrieved from www.english.metro.tokyo.lg.jp/w/081-101-003873.
- Met Office (2021). UK Climate Projections 2018. Retrieved from www.metoffice.gov.uk/research/approach/collaboration/ukcp.
- Water UK (2017). Water resources long term planning framework. London: Water UK. Available at: www.water.org.uk/sites/default/files/wp/2018/11/WaterUK-WRLTPF_Final-Report_FINAL-PUBLISHED-min.pdf.
- NHS Sustainable Development Unit (2009). Saving carbon, improving health: NHS carbon reduction strategy for England. Available at: www.england.nhs.uk/greenernhs/wp-content/uploads/sites/51/2021/02/NHS-Carbon-Reduction-Strategy-2009.pdf.
- NHS Estates (2004). Health Technical Memorandum 07-04: Water management. London: The Stationery Office. Available at: www.england.nhs.uk/wp-content/uploads/2021/05/HTM_07-04_Final.pdf.
- Shah FA, Shyam A. The Evolution Of Surgical Hands Anti-Sepsis: From Scrub To Rub. Journal of Orthopaedic Case Reports. 2025;15(02):1-3.
- NICE (2008). Infection control: Prevention of healthcare-associated infections in primary and community care. London: NICE.
- Water Use Calculation. Available at: www.nyc.gov/assets/dep/downloads/pdf/environment/education/sewers-activity-water-use-calculation.pdf.
- Potgieter MSW, Faisal A, Ikram A, Burger M. Water-wise hand preparation - the true impact of our practice: A controlled before-and-after study. S Afr Med J. 2020;110(4):291-5.
- Gasson S, Solari F, Jesudason EP. Sustainable Hand Surgery: Incorporating Water Efficiency Into Clinical Practice. Cureus. 2023 Apr;15(4):e38331.
