GIRFT national guidelines for cauda equina syndrome (CES) – a guaranteed success?
By Andreas Conte
Final year medical student at Kings Cross College, London
|
This is the winning essay from the 2024 BOA Medical Student Essay Prize Entrants were asked to write a Quality Improvement Project (QIP) on the following topic: 'With the changing demographics and working practices within T&O how can we sustain the work force and standards of care currently provided within the NHS?' |
Introduction
Cauda equina syndrome (CES) is a surgical emergency driven by compression to the spinal roots1. Definitive treatment is urgent surgical decompression. Delays in diagnosis or surgical treatment can lead to lower limb paralysis, bowel and bladder incontinence, sexual dysfunction, and chronic pain.
GIRFT National Guidelines specify that patients with red flag symptoms for CES require an “emergency MRI as soon as possible, certainly within 4 hours of request”2, however, a recent audit at Medway Maritime Hospital showed that the mean time from presentation to MRI was 10 hours (median 6 hours). The primary aim of this QIP was to reduce the time from Emergency Department (ED) presentation to MRI scan.
Investigating the problem
A qualitative thematic analysis of patient and staff experience was conducted to better understand the reasons behind these delays. Six patients with lived experience of CES, and five healthcare providers (ED triage nurse, ED doctor, orthopaedic on-call, radiologist, radiographer) were interviewed. After coding and thematic analysis, a fishbone cause analysis (Figure 1) was constructed to identify possible targets for interventions.
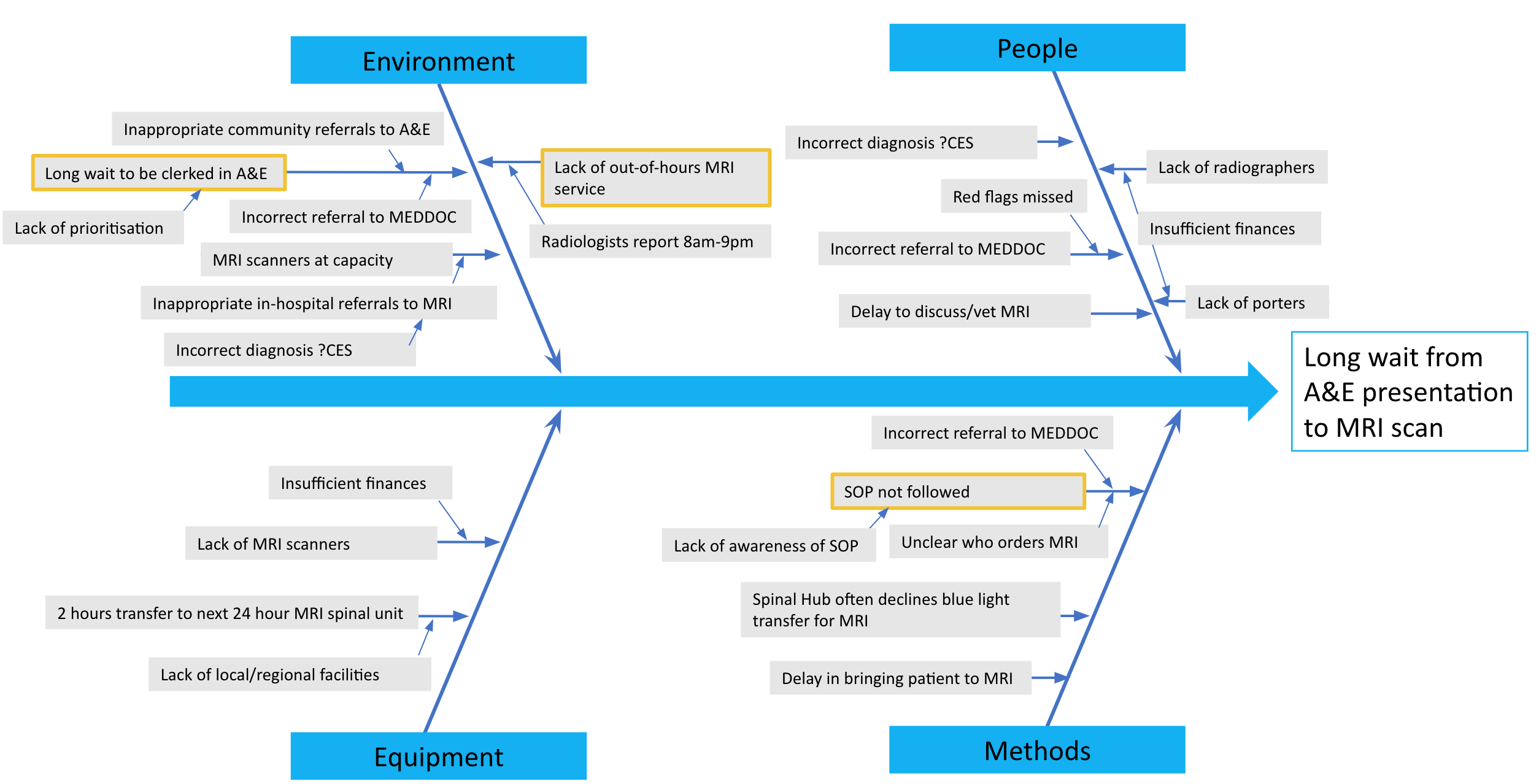
Figure 1: Fishbone cause analysis for delays in obtaining an MRI for suspected CES.
The key themes derived from the healthcare providers were: a) medical professionals often misunderstand CES, b) there is uncertainty between ED and Orthopaedics as to who is responsible for the patient, c) there is widespread frustration at the lack of out-of-hours MRI, with the scanners only operational from 8am-8pm. Amongst patients: a) they experience poor communication, b) have difficulties in accessing care, c) experience pain throughout their journey. Figure 2 shows the struggles that ‘Gareth’, an award-winning amateur cyclist, faced when accessing care for his back pain.
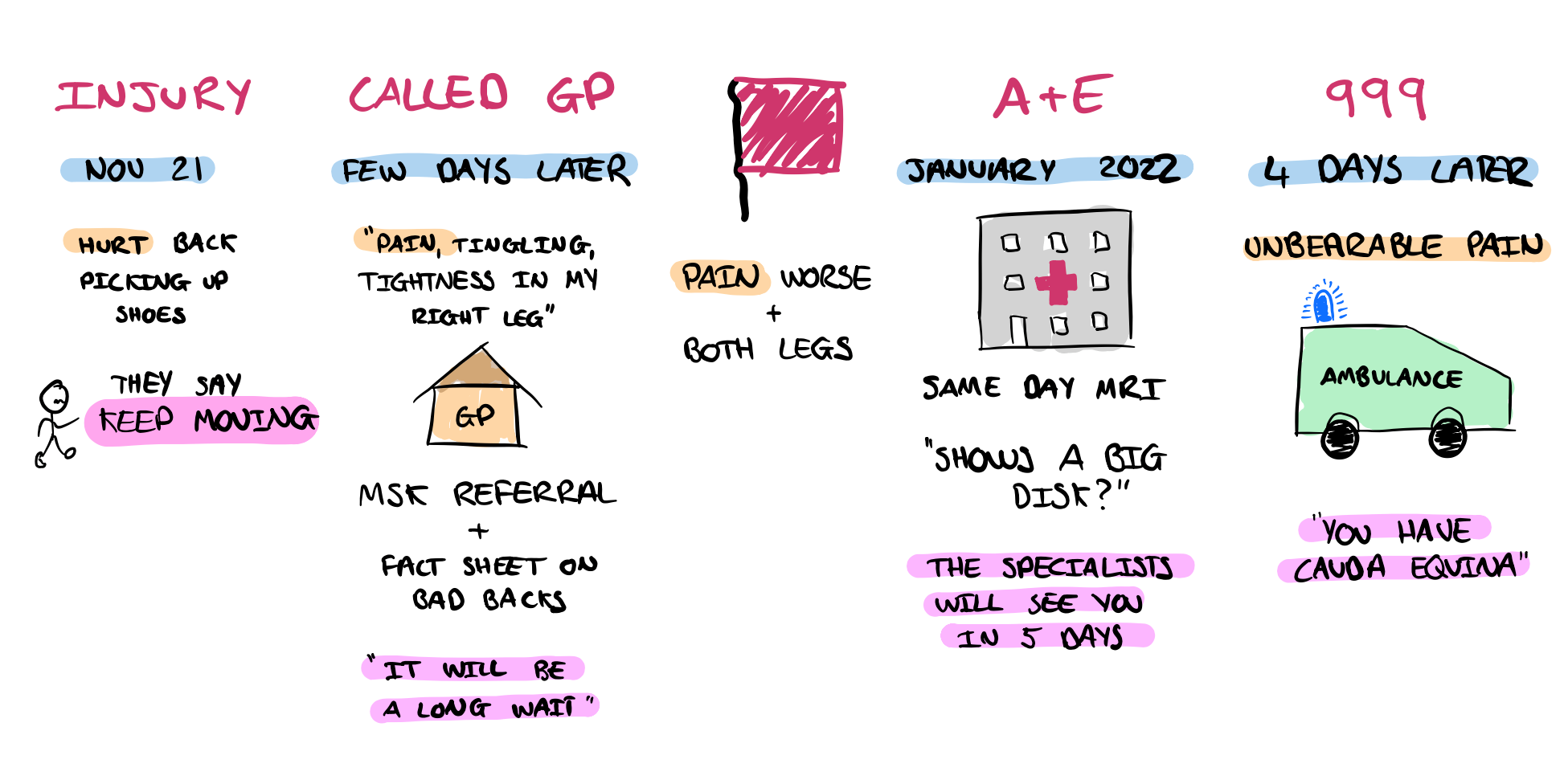
Figure 2: A patient journey map, from injury to diagnosis.
Creating solutions
Given the inconsistency with which these patients are managed at Medway, it was believed that the implementation of a GIRFT standard operating procedure (SOP) would streamline the journey from ED presentation to MRI scan, as well as define patient ownership between ED and Orthopaedics. Figure 3 highlights the old, inconsistently used SOP, and the new, streamlined GIRFT SOP.
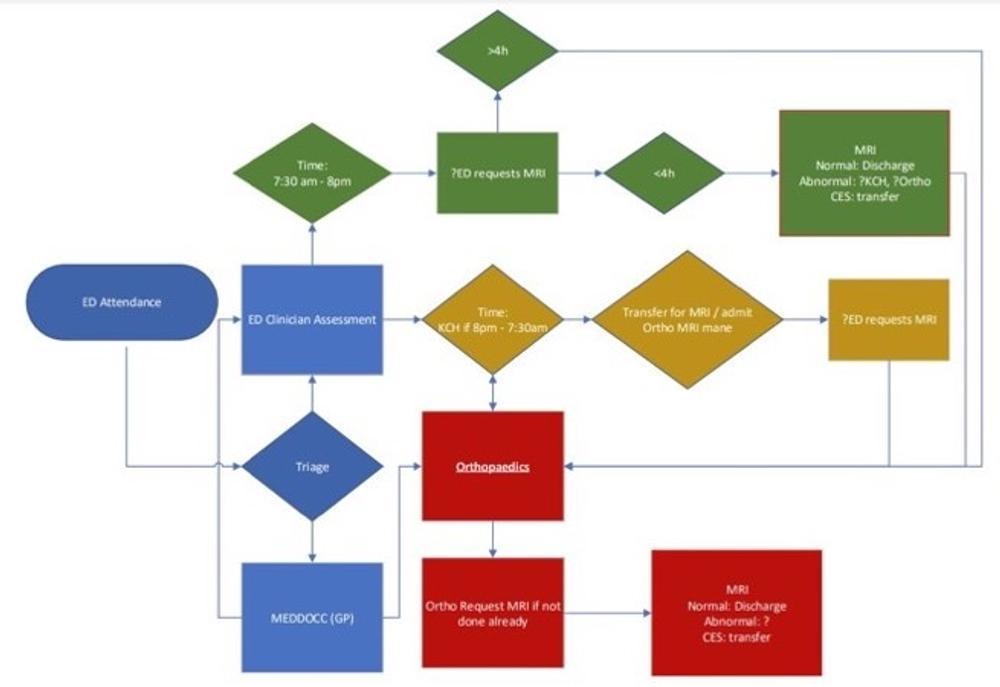
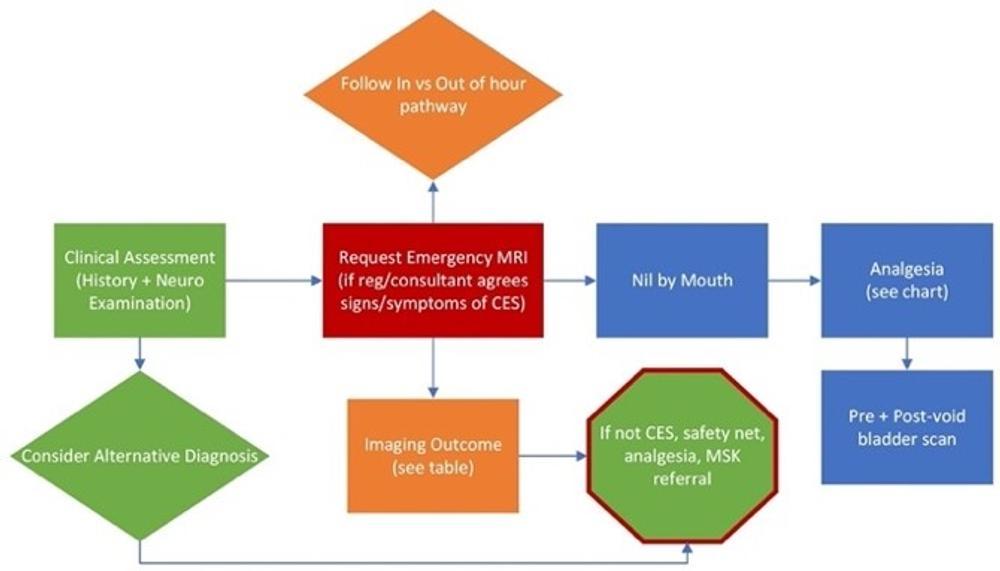
Figure 3: The old suspected CES SOP (top) and the new, GIRFT suspected CES SOP (bottom).
In order to address the misunderstandings of CES amongst clinicians, additional focus on clinical education was prioritised within the ED - covering the red flags, history taking and examination techniques for CES.
PDSA cycles
This QIP worked through three PDSA cycles. The first cycle focused on MDT improvement – raising awareness of the delays amongst Orthopaedics, Radiology, and ED to promote internal improvement. The second cycle focused on GIRFT SOP implementation. The third cycle focused on SOP promotion with posters throughout the ED, presentations at Board Rounds and the Hospital Grand Round, and clinical education within the ED. Figure 4 shows the poster that was hung throughout the ED, covering the new SOP, red flags, steps to order an MRI, and management pathway following MRI results.
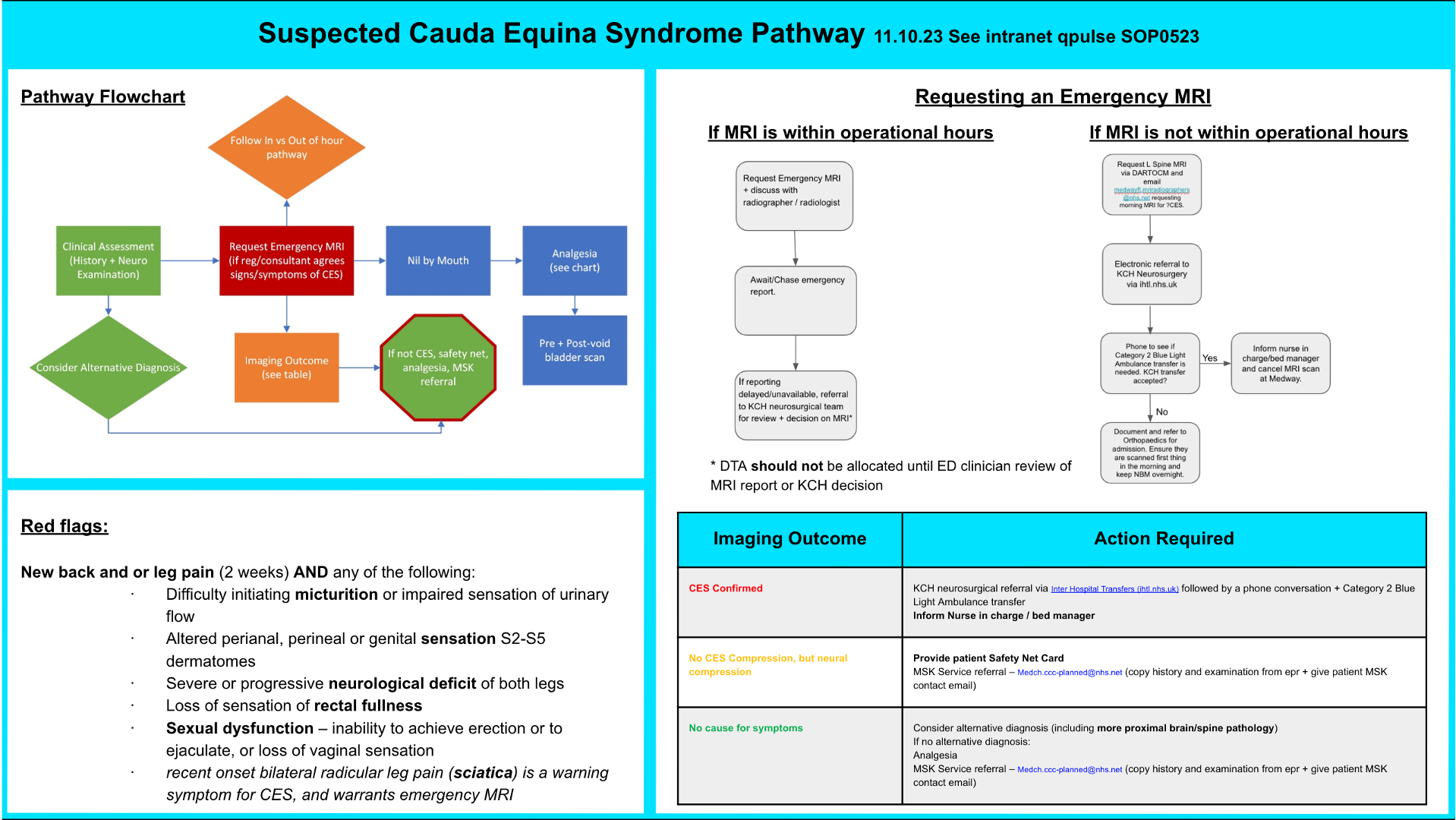
Figure 4: The suspected CES pathway poster hung throughout the ED department.
Measuring change
Each cycle included approximately 30 patients. Data were collected retrospectively on their time of arrival in ED to clerking, analgesia and MRI scan. Data were also collected on the percentage of MRI requests that satisfied the red flag criteria for MRI scan.
Results
Whilst Medway was able to achieve the GIRFT target of four hours between MRI request and MRI scan, this QIP was unable to reduce the time to MRI scan completion (Figure 5). Medway fails to provide an emergency same-day MRI for around half of patients. Up to 20% of MRI requests did not satisfy red flag criteria for MRI scan, but there was a trend of improvement throughout PDSA cycles (Figure 5). Finally, the median time from ED presentation to MRI scan across PDSA 2 and 3 was nine hours, with a concerning 3-hour delay between clerking and MRI request (Figure 6).
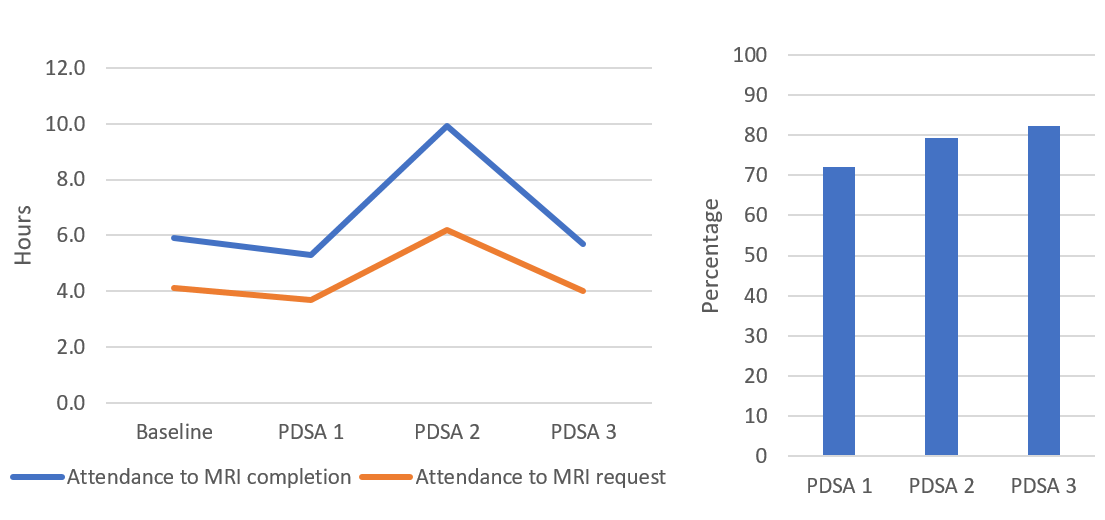
Figure 5: Median time from attendance to MRI request and MRI scan (left) and percentage of MRI requests that satisfy red flag criteria for MRI scan (right).
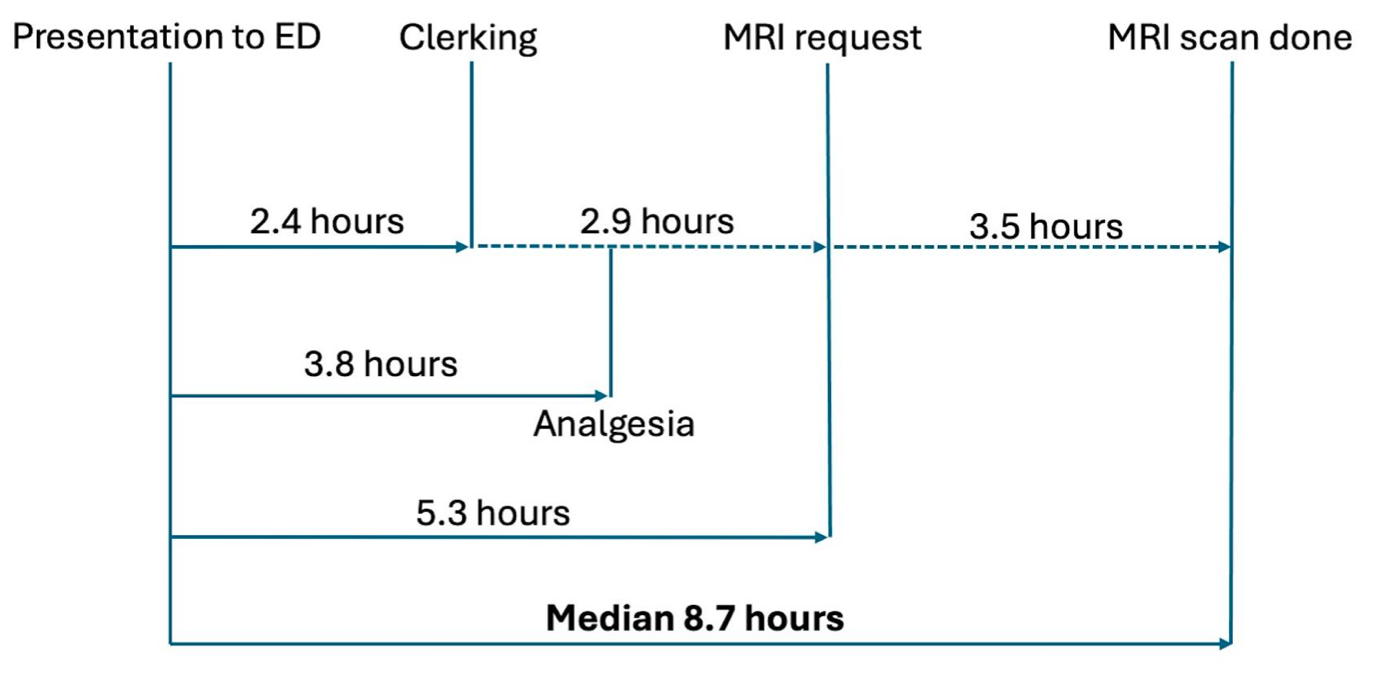
Figure 6: Run chart from ED presentation to MRI scan, combining data from PDSA 2 and 3.
Going forward
This QIP was successful in implementing GIRFT National Guidelines, however, these did not reduce the time from ED presentation to MRI. The key learning point from this project was that top-down National Guidelines are only one part of the puzzle in driving change. In order to be successful, they must be adjusted and shaped to the local context3,4.
Two root causes have been identified for the continued delay to MRI request. Firstly, the new SOP is not being followed. There is a long delay from clerking to MRI, and a large proportion of imaging requests are unnecessary. To combat non-adherence to the SOP, a specific ED CES audit project with regular teaching has been launched, with the aim of reducing the time from clerking to imaging request. Moreover, there will be a new standardised CES MRI request form with the red flags to highlight the inclusion criteria for MRI scan.
The second root cause for continued delay is the restriction in imaging hours. Figure 7 shows the time of presentation of 81 patients over PDSA cycles 1-3. Only patients that presented between 3am and 3pm were likely to have a same day emergency MRI. The other patients (43/81) were delayed to the next day, requiring overnight admission. By extending scanning by 2 hours from 8pm to 10pm, performance could be improved by 60%, with only 27/81 patients requiring overnight admission. In response to this QIP, the hospital is now considering extending MRI hours, to bring Medway closer to GIRFT National Guidelines2 which specify the need for 24-hour MRI provision.
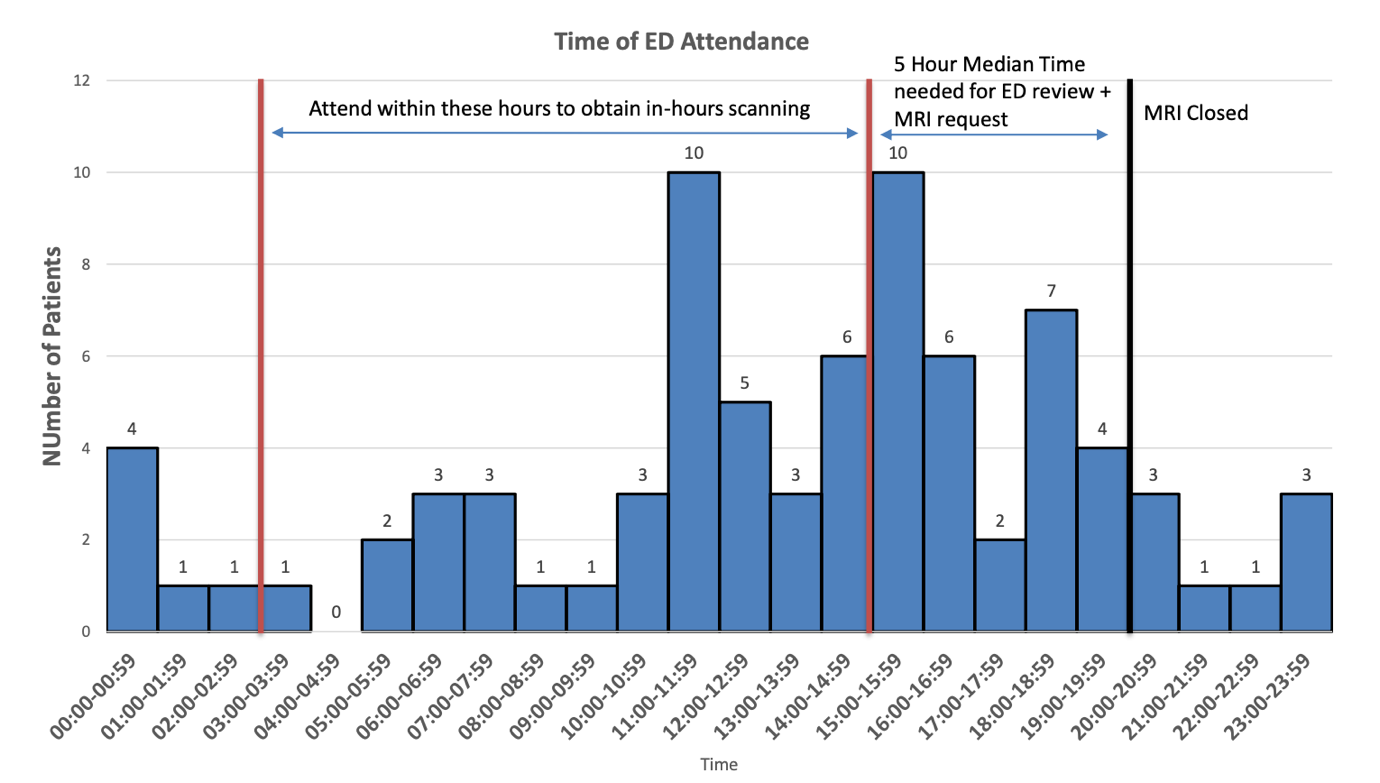
Figure 7: Time of ED attendance and clerking for patients across PDSA cycles 1-3, a demand and capacity assessment.
Challenges and limitations
The primary challenge faced by this QIP was the multi-departmental causes of the delays. An interdisciplinary approach was needed to tackle this issue, creating shared ownership of the problem between Orthopaedics, Radiology and ED. Despite no reduction in time to MRI scan, all teams remain committed to clinical education, the new SOP, and extension of imaging hours.
Two limitations may have impacted the results of this QIP. The first was that PDSA 2 and 3 occurred during junior doctor strikes, likely delaying a patient journey through ED. Secondly, each cycle had large differences in times of ED presentation. PDSA 1 had the shortest time to MRI, but the earliest median time of ED presentation (11.43). PDSA 2 had the longest time to MRI, and the latest median time of ED presentation (16.27). Further PDSA cycles should include larger number of patients to reduce such effects.
References
- Lavy C, Marks P, Dangas K, Todd N. Cauda equina syndrome-a practical guide to definition and classification. Int Orthop. 2022;46(2):165-9.
- GIRFT (Getting it Right First Time). Spinal Surgery: National Suspected Cauda Equina Syndrome (CES) Pathway. 2019 [Accessed 22/02/2024]; Available from: https://gettingitrightfirsttime.co.uk/wp-content/uploads/2023/10/National-Suspected-Cauda-Equina-Pathway-UPDATED-V2-October-2023.pdf.
- Bergman DA. Evidence-based guidelines and critical pathways for quality improvement. Pediatrics. 1999;103(1 Suppl E):225-32.
- Sigsbee B, Bever CT Jr, Jones LK Jr. Practice improvement requires more than guidelines and quality measures. Neurology. 2016;86(2):188-93.
