COVID-19 second wave, avoid service and training dislocation
By Ahmed Fadulelmola, Rob Gregory, Catherine Molyneux, Gavin Gordon, Fiona Smith and Andrew Jennings
University Hospital of North Durham, County Durham & Darlington NHSF
Corresponding author e-mail: [email protected]
Published 05 November 2020
Introduction
Since the latter part of 2019, a novel virus, SARS-CoV-2 (COVID-19) originating in China has been the cause of a global pandemic. In the UK, 2020 COVID-19 mortality rate had surpassed the annual deaths from stroke or lung cancer in 20191. The pandemic had led to change in practise and dislocated different aspects of elective services, and training. The British Orthopaedic Association (BOA) has published guidance for Management of patients with urgent orthopaedic conditions and trauma during the coronavirus pandemic and urges pragmatism2. A second wave will cause further effect on orthopaedics elective services and collateral damage to training3.
Hip fractures have an estimated incidence of 4.5 million cases per year worldwide and 80,000 per year in the UK4,5. The last estimates of UK number of cases for 2020 were 101,000 patients6. This injury necessitates hospital admission, and consequently makes this group particularly prone to nosocomial COVID-19 infection.
Hip fractures are associated with increased mortality. We found that the mortality figures increased when hip fractures are associated with COVID-19 infection7. We have postulated that surgery post COVID-19 infection may lead to a third hit resulting in increased mortality. There is emerging evidence suggesting increased mortality rate in orthopaedics injuries combined with COVID-19 infection8.
It is reported that COVID-19 affects groups in close contact such as hospitalised patients9. However, there is no published evidence on the effect of hospital acquired COVID-19 infection in hip fracture patients.
The aim of this study is to analyse the effect of hospital transmission of COVID-19 infection on early hip fracture mortality and presents an admission protocol for emergency and elective orthopaedics cases in the case of second COVID-19 wave.
Patients and methods
We have retrospectively reviewed all adult hip fractures admitted to the University Hospital of North Durham and Darlington Memorial Hospital in March 2020 and April 2020. Demographic data, the Nottingham Hip Fracture Score, the Charlson comorbidity index, and Cognitive state (as evaluated using the Abbreviated Mental Test Score10) were documented. COVID-19 had been diagnosed according to the national and local guidelines, using reverse transcriptase polymerase chain reaction (SARS-CoV-2 RdRp RT-PCR) of throat swap samples. All patients had received low molecular weight heparin (Enoxaparin forty milligrams) to prevent thromboembolic event. Patients underwent surgery when it deemed safe following multi-disciplinary consultant review by Orthopaedics, care of Elderly, and anaesthetics.
The primary outcome measure was mortality associated with COVID-19 infection in hip fracture patients. Secondary outcome measures where medical complications (myocardial infarction, deep vein thrombosis, pulmonary embolism, and pneumonia), surgical complications (infection, mechanical failure, dislocation, and fracture), radiological appearance and laboratory results relating to diagnosis and treatment of COVID-19.
We have epidemiologically investigated the risk of hospital transmission of COVID-19 in the orthopaedics ward. The wards in both hospitals are labelled for COVID-19 infection status following a traffic light pattern. Red is COVID-19 positive cases isolation area, Amber is COVID-19 suspected cases ward, and Green is COVID-19 free area. The highlighted cases were investigated in terms of their placement within the ward during the period of increased inpatient activity with COVID-19, and at a time when national guidance of prevention of nosocomial transmission was at it its infancy.
Statistical analysis
The results were analysed to assess mortality associated with COVID-19 infection. Normally distributed data is presented as mean value and standard deviation. Kolmogorov-Smirnov test was used for normality of distribution. Pearson Chi-square, Student t test, and binomial test, were used to detect the differences between COVID-19 positive and negative patients. Statistical Package for social Science (SPSS, version 24.0 IBM) had been used.
Results
75 patients presented with hip fractures during the study period (41 patients in Durham and 34 cases in Darlington). Table 1 and 2 summarise the patients’ characteristics and laboratory findings. There was no statistical difference in the mean age between the two units (84.1 and 82.8 years in Durham and Darlington, respectively, p = 0.07). All the hip fractures (n = 75) were due to low velocity injury. The COVID-19 infection rate was 26.7% (n = 20, 13 patients in Durham and 7 cases in Darlington). There was a significant difference of mortality rate in Durham (n = 11/41, 26.8%) compared to Darlington (n = 3/34, 4%), p = 0.04. There was a significant difference of mortality rate in COVID-19 positive group (n = 10, 50%) compared to COVID-19 negative group (n = 4, 7.3%), p = 0.003. Univariate analysis showed there was statistically significant effects of COVID-19 positive infection on the mortality difference between the two hospitals F = 4.05, p = 0.04. Two-way ANOVA showed there was no statistically significant effects of gender, socioeconomic status and the Charlson co-morbidity index as confounders on mortality, p = 0.074. The average time of death was 15.9 days post admission (range 7-29). The average time of death was 15.9 days post admission (range 7-29). The mean time from admission to surgery was 38.4 hours and 40.1 hours, in Durham and Darlington groups, respectively, p = 0.15.
30.8% (n = 4) and 67.5 % (n = 5) contracted the COVID-19 in the community and 69.2% (n = 9) and 28.5% (n = 5) developed symptoms after hospital admission in Durham Hospital and Darlington Hospital, respectively. In a month period the orthopaedic ward was amber in 15 days (50%) compared to 4 amber days (13%) in Durham and Darlington, respectively. Seven out of thirteen patients (53.8%) were identified as having significant close contact (same bay) with COVID-19 positive patient in Durham hospital.
|
|
Durham n = 41 |
Darlington n = 34 |
|
Age (mean) |
84.1 years |
82.7 years |
|
Gender Female Male |
27 (65.9%) 14 (34.1%) |
26 (76.5%) 8 (23.5%) |
|
Mortality Yes No |
11 (26.8%) 30 (73.2%) |
3 (8.8%) 31 (91.2%) |
|
COVID-19 Positive Negative |
13 (31.7%) 28 (68.3%) |
7 (20.6%) 27 (79.6%) |
|
Fracture classification Intra-capsular Extra-capsular |
27 (65.9%) 14 (34.1%) |
23 (67.6%) 11 (32.4%) |
|
Time from admission to surgery (mean) |
37.4 hours |
39.8 hours |
|
Operations Cemented hemiarthroplasty Uncemented hemiarthroplasty Dynamic hip screw Intra-medullary nail THR Conservative |
2 (61.0%) 1 (2.4%) 11 (26.8%) 1 (2.4%) 2 (4.8%) 1 (2.4%) |
21 (61.8%) 0 (0%) 6 (17.6%) 4 (11.8%) 1 (2.9%) 2 (5.9%) |
|
Type of anaesthesia a Spinal General |
17 (41.5%) 23 (56.1%) |
18 (52.9%) 14 (41.2%) |
|
Complications Surgical b Medical c |
1 (2.4%) 1 (2.4) |
0 (0%) 0 (0%) |
|
Place of residence Own home Institution |
33 (80.5%) 8 (19.5%) |
18 (52.9%) 16 (47.1%) |
a three patients were managed conservatively and did not need anaesthesia.
b periprosthetic fracture.
c Myocardial infarction.
THR: Total Hip Replacement.
|
Mean |
Durham n = 41 |
Darlington n = 34 |
|
CRP |
29.3 |
46.5 |
|
WCC |
10.9 |
12.1 |
|
Lymphocytes count |
1.3 |
0.9 |
|
Pre-operative haemoglobin g/l |
119.8 |
121.3 |
|
Post-operative haemoglobin g/l |
99.9 |
103.8 |
|
Haemoglobin drop post-operative g/l |
19.9 |
17.45 |
CRP: C Reactive Protein
WCC: White Cell Count (x 109 cells/litre)
Discussion
This study presents the first evidence of the effect of COVID-19 hospital risk of transmission on the early mortality of patients presented with hip fractures. We have reported high 30-days mortality among COVID-19 positive patients (50%)7. Recent estimates of COVID-19 related fatality in patients older than 60 years ranges from 8% to 36%11,12. The average time to death from admission was 15.9 days in our study. Similar findings have been reported from China with mean time from disease onset to death of 17.8 days13. Mi et al. reported ten patients who died due to COVID-19 associated with orthopaedic fractures in two months in Wuhan province in China, six of them presenting with hip fractures14.
Five (38.4%) cases of definite nosocomial infection were identified with another two patients (15%.3) identified as having possible nosocomial infection in Durham. In further details, two were together in one bay, two in a second bay, and three in a third bay. All of the seven patients were COVID-19 negative on admission. There appear to have been two probable and one possible cluster of cases on the orthopaedics ward. All three potential clusters occurred after visiting was suspended. The relatively long incubation period of COVID-19 infection and the test result delay meant that patients had usually been diagnosed after admission to the orthopaedics ward making clinical detection of clusters difficult. Sikkema et al. reported three hospital clusters with suggested inter hospital transmission15. In a review from UK it is found that 66 out of 435 COVID-19 positive cases were reported to be nosocomial16. Based on SARS (Severe Acute Respiratory syndrome) virus studies the major routes of transmission of COVID-19 virus are thought to be respiratory droplets and direct contact17. We have proposed two pathways for patients presenting with orthopaedics problems both acute and elective in order to reduce the risk of hospital transmission, maintaining COVID-19 free wards, and decrease COVID-19 hospital clusters (Figure 1, and 2).
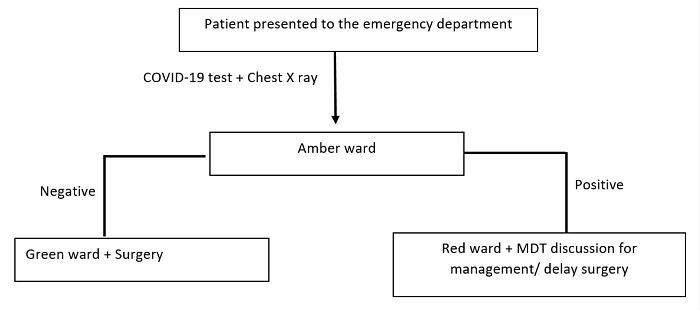
Figure 1: Proposed pathway for acute orthopaedics injuries.
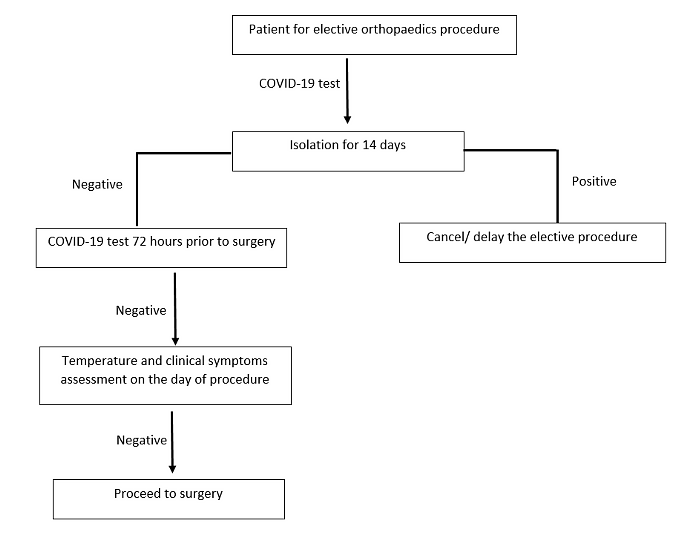
Figure 2: Proposed pathway for elective orthopaedics admissions.
On the basis of our study, hospital acquired COVID-19 infection is a potential hazard with risk of devastating sequalae in orthopaedics. Due to the risk of second infection wave, we have adopted a protocol of COVID-19 testing and Chest X ray, for all patients presenting acute orthopaedics injury in our unit and proposed two pathways to manage acute and elective orthopaedics cases in relation to COVID-19 infection. We believe this will help in reduction of potential clusters and hospital transmission.
Conclusion
- Hospital acquired COVID-19 infection in orthopaedics causes increased mortality and can lead to disruption of elective orthopaedics and training.
- Splitting acute and elective cases to two pathways would lead to reduction of the risk of COVID-19 hospital infection and facilitate better patients care and training quality.
- Pre-operative self-isolation, COVID-19 testing, and chest X ray are safe tools to reduce COVID-19 hospital transmission.
References
- The King's Fund (2020). Deaths from Covid-19 (coronavirus): [cited 12 September 2020]. Available at: https://www.kingsfund.org.uk/publications/deaths-covid-19.
- British Orthopaedic Association (2020). BOAST- Management of patients with traumatic injuries and urgent orthopaedic conditions requiring inpatient care during the coronavirus pandemic. Available at: https://www.boa.ac.uk/uploads/assets/ee39d8a8-9457-4533-9774e973c835246d/4e3170c2-d85f-4162-a32500f54b1e3b1f/COVID-19-BOASTs-Combined-FINAL.pdf.
- Megaloikonomos P, Thaler M, Igoumenou V, Bonanzinga T, Ostojic M, Couto A, et al. Impact of the COVID-19 pandemic on orthopaedic and trauma surgery training in Europe. Int Orthop. 2020;44(9):1611-9.
- Gulleberg B, Johnell O, Kanis JA. Worldwide projections for hip fracture. Oteoprosos Int. 1997;7:407-13.
- Parker M, Johnasen A. Hip fracture. BMJ. 2006;333:27-30.
- Giannoulis D, Calori G, Giannoudis P. Thirty-day mortality after hip fractures: has anything changed?
Eur J Orthop Surg Traumatol. 2016;26(4):365-70.
-
Fadulelmola A, Gregory R, Gordon G, Smith F, Jennings A. The impact of COVID-19 infection on hip fractures 30-day mortality. Trauma. August 2020.
- Price A, Shearman A, Hamilton T, Alvand A, Kendrick B. 30-day outcome after orthopaedic surgery in patients assessed as negative for COVID-19 at the time of surgery during the peak of the pandemic. Bone & Joint Open. 2020;1(8):474-80.
- Rothe C, Schunk M, Sothmann P, Bretzel G, Froeschl G, Wallrauch C, et al. Transmission of 2019-nCoV Infection from an Asymptomatic Contact in Germany. N Engl J Med. 2020;382(10):970-1.
- Jain N, Guyver P, McCarthy P, Sarasin S, Rouholamin N, McCarthy M. Use of the Abbreviated Mental Test Score by junior doctors on patients with fractured neck of femur. Arch Orthop Trauma Surg. 2008;128(2):235-8.
- Banerjee A, Pasea L, Harris S, Gonzalez-Izquierdo A, Torralbo A, Shallcross L, et al. Estimating excess 1-year mortality associated with the COVID-19 pandemic according to underlying conditions and age: a population-based cohort study. Lancet. 2020;395(10238):1715-25.
- WHO (2020). Report of the WHO-China Joint Mission on coronavirus disease 2019 (COVID-19). Available at: https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf.
- Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507-13.
- Mi B, Chen L, Xiong Y, Xue H, Zhou W, Liu G. Characteristics and Early Prognosis of COVID-19 Infection in Fracture Patients. J Bone Joint Surg Am. 2020;102(9):750-8.
- Sikkema RS, Pas SD, Nieuwenhuijse DF, O'Toole A, Verweij J, van der Linden A, et al. COVID-19 in health-care workers in three hospitals in the south of the Netherlands: a cross-sectional study. Lancet Infect Dis. 2020;20(11):1273-80.
- Rickman HM, Rampling T, Shaw K, Martinez-Garcia G, Hail L, Coen P, et al. Nosocomial transmission of COVID-19: a retrospective study of 66 hospital-acquired cases in a London teaching hospital. Clin Infect Dis. 2020 Jun 20. [Epub ahead of print].
- Lee N, Hui D, Wu A, Chan P, Cameron P, Joynt GM, et al. A major outbreak of severe acute respiratory syndrome in Hong Kong. N Engl J Med. 2003;348(20):1986-94.
