Coronavirus (COVID-19): My experience of testing positive
By Kathryn S S Dayananda
Specialty Trainee Trauma and Orthopaedic Surgery, Wales Deanery
Cardiff and Vale University Health Board
Published 16 April 2020
As a patient
After finishing the morning hand trauma list, I sat in the doctor’s office with my colleague, who was known to be high-risk. We were discussing the options on how to record and publicise the exemplary and timely changes we felt our unit had made in order to prepare for the coronavirus pandemic.
I started to develop some nasal congestion and headache and decided to head home slightly earlier than usual. During the course of my 20-minute commute the headache progressed to such an extent that I went straight to bed. Within an hour I was feverish with flu-like symptoms. It was clear I was ill-was it the coronavirus or something else?

I was desperately worried about my colleague. I messaged him urgently to let him know. I felt so awful for sitting with him despite distancing as much as possible. My symptoms progressed rapidly.
I emailed, as per our local department guidelines, to enquire about testing and began the isolation process immediately. My husband kept away, slept in the spare room and used a separate bathroom. I had lost my appetite and had no energy to get up. I stayed in bed for 3 days. Gradually I developed a cough, although this wasn’t severe, and completely lost my sense of smell. I felt extremely achy and lethargic, suffered a vasovagal episode, and was short of breath despite minimal exertion. My resting heart rate had almost doubled and I was unable to undertake any activity in my home.
Gradually over the following 7-10 days I began improving, spending the majority of my time on the sofa resting. I received the call from Public Health Wales notifying me that my test was positive and wishing me a swift recovery.
As a colleague
This was my longest period of absence for sick leave to date having only had a total of 3-4 days off since qualifying in 2012. Although essential for my health and the health of others, being off work did not come easily or naturally to me.
Prior to receiving my swab results I blamed myself for being lazy and inefficient with my time. I was frustrated at not being able to help out about the house or in work. I was exasperated by my inability to concentrate on anything.
Most of all I worried about the staff, patients and public I could have infected without realising, especially my high-risk team-mate and friend.
I felt extremely guilty that others would have to step into my on-call slots and other clinical commitments. I would say things like “I’m a team-player and I should be in work helping my friends and patients”.
As I began improving, I started to feel the cabin fever effects of isolation, yearning to get back to ‘normality’ and the dynamic hospital environment.
Throughout my illness and return to work I have been fully supported by Consultants, colleagues and management. I returned directly onto the nightshift and the realisation that the hospital would be a very different place to how I left it soon dawned on me. I quickly caught up with a detailed Consultant lead handover. I found it reassuring to have at least a degree of immunity against the virus. I was grateful to be back. I was able to interact with and support colleagues, help those in need, and do my part in the National fight against the invisible enemy.
|
“I hate being at home when everyone else is struggling at work” “I’d like to try and come for hand clinic Friday. Fingers crossed. And also get back to helping with on calls, because I hate being such a waster.” Messages sent from me to our rota co-ordinator colleague while off |
As a Specialty Trainee Care Provider
When the news came that all elective operating would be cancelled, the gravity of the situation dawned on me.
Within days our department had made huge logistical changes to the delivery of trauma service provision across Cardiff and Vale University Health Board. With strong leadership, tireless efforts from our Consultants and immense team-work, the trauma theatre, fracture clinic and trauma ambulatory care unit (TACU) were re-distributed to our elective unit on a separate site. Spinal, paediatric and polytrauma remained at our tertiary referral unit. This enabled a degree of containment of COVID-19 in the initial period, releasing beds, and supporting a restructuring of the staff rota. Two separate site rotas were devised to prevent cross contamination from staff. It also compensated for the redeployment of non-consultant staff at all levels. These changes were encouraging for all trainees. It demonstrated departmental unity and care for each other. The creation of wellbeing boxes confirmed that our departments approach to tackling COVID-19 would be compassionate and charitable. It was reassuring to receive such top-down support.
We all had three key concerns; patient and personal safety and training. Our Training Programme Director (Mr Khitish Mohanty) gave thorough and clear advice in line with national recommendations regarding ARCPs and job rotations, which reassured us all. Virtual teaching was delivered where possible. Copious access to training sessions such as donning and doffing, medical management of the acutely unwell patient suffering COVID-19, and improving practical and logistical skills in ward management have all been made readily available. A virtual mindfulness session has equipped us with strategies to remain composed in times of distinct uncertainty.
The cohesive nature of the entire department and outstanding links with our orthogeriatric team have been second-to-none. It has made coming to work during these unprecedented times as stress free as possible.
Advice for colleagues
We are here to help others when they can no longer take care of themselves. You must therefore make it your priority to look after yourself. Although for many of us it will go against our nature, you must take full rest when you need, for as long as you need. This can only be dictated by the individual. You have a responsibility to do this for yourself, for your colleagues and for your patients.
Don’t be fearful of accepting you don’t know. As well as providing trauma care, we are here to support specialties we have limited experience in. Many of us will be asked to perform tasks we are out of practice with or are unfamiliar to us. Be humble and ask for guidance and / help. Like-wise you must go above and beyond to help others in your team, hospital and wider community when they need, ideally before they need to ask.
Keep active. It will protect your mental and physical health.
Try to be in-tune with your emotions. If you identify with increasingly upset feelings do not see this as failure. With increasing numbers of patients, staff, friends and family succumbing to this disease it is natural. Tackle them in the way that suits you, and if you’re not sure how to do this (none of us have lived / worked through a pandemic before) seek advice.
Practice what you preach and do not take part in any unnecessary or risky activities. Avoid any non-essential travel.
And if in doubt, “wear sunscreen”. (Baz Luhrmann)
We wish you all good health and safe practising. From all at the T&O Department in Cardiff and Vale UHB.
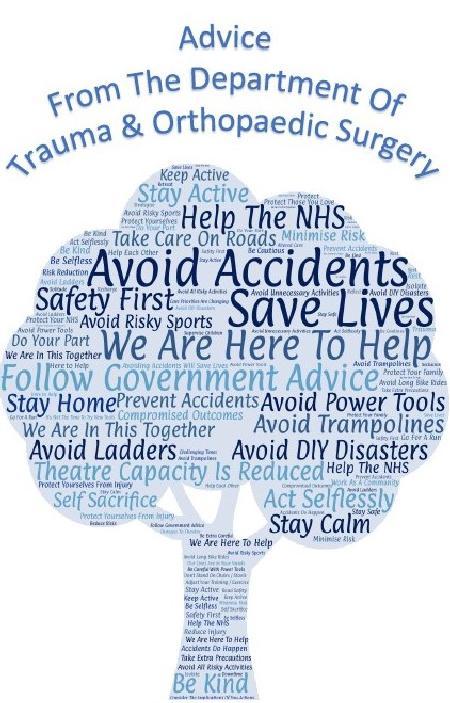
Collated departmental advice for the public