A commentary on Prone Position Plexopathy during the COVID-19 pandemic
by Tom Quicka,b, Hazel Browna,ba Peripheral Nerve Injury Unit, Royal National Orthopaedic Hospital, Stanmore, UK
b Centre for Nerve Engineering, UCL, London, UK
Corresponding author email: [email protected]
Published 10 May 2020
The COVID-19 pandemic has led to a large cohort of patients across the country requiring prolonged ventilation. Many of these are being managed for long periods of time in a prone position. There are many risks of proning patients, including those of injury sustained inadvertently due to the positioning. Methods to avoid pressure sores and ocular damage are well understood1. Concerns regarding injury to the brachial plexus have created some discussion. In recent weeks our national nerve injury unit has received numerous queries regarding the rationale for the proning posture and how best to assess and manage patients, who upon regaining consciousness, have altered upper limb neurology or a Prone Position Plexopathy (PPP).
The UK guidelines2 recommend an alternating ‘swimmers position’ for the upper limbs when positioning an unconscious patient; the rationale for this is not well documented. However, the literature shows that there is little variance within the guidelines across countries,3-5. The one arm abducted one adducted - ‘swimmers position’ is one which we have avoided using in operating theatres; favouring both arms down or both arms slightly abducted with the head well supported in the anatomic neutral position6. Asymmetrical arm positions risk a traction injury to the plexus on the side of the adducted arm if the head is excessively laterally flexed away from that side.
Ergonomically the situation in critical care is different to that of theatre. The head cannot easily be placed facing anatomically forward (into the bed) and is thus rotated. The rotation advised within the swimmers position (with face towards the abducted arm) means that lateral flexion away from the adducted arm is bio-mechanically impossible. Anatomically this opens up the neural foramen on the adducted side; theoretically relieving local pressure on the emerging nerve roots.
Applying the principles of tissue biomechanics and injury mechanisms (which are well understood from animal work and cadaveric studies) we understand that the major causes of injury in closed nerve injury are compression and traction. In our clinical practice we often see plexus injuries in those who have maintained a prolonged recumbent posture. The reasons for this include: intoxication, inability to rise from the ground following a fall, physical entrapment or unconsciousness. Once again these patients are dissimilar to the presentation of those in the critical care setting; often demonstrating multiple end stage complications such as compartment syndrome, rabdomyolysis, skin necrosis and dehydration.
The principles of direct nerve injury are best understood as damage to different anatomical regions of the brachial plexus. The supra-clavicular, retro-clavicular and infra-clavicular areas of the plexus are prone to injury in differing positions. Combining this knowledge with the bio-mechanical risk of injury from traction/compression allows the formulation of recommendations to avoid such injuries when placing and maintaining patients in a prone posture (Figure 1).
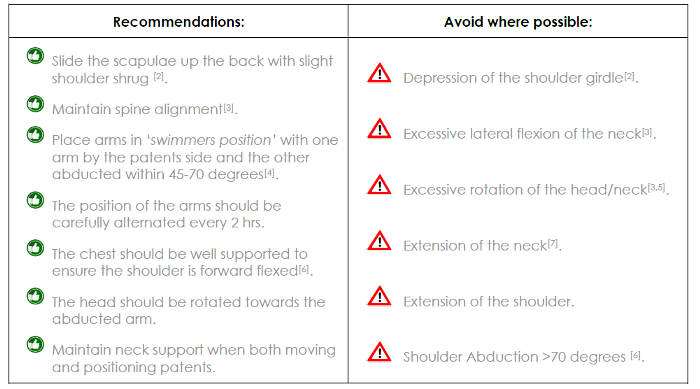
Figure 1. Recommendations taken from the Royal National Orthopaedic, Peripheral Nerve injury Unit by the authors7.
In summary, when positioned prone with the head rotated it is important that the cervical spine is kept in neural or slightly flexed and never extended8. Care must also be taken to maintain neutral alignment of the cervical spine (not laterally flex) when repositioning from one rotation to the other9,10.
In the ‘swimmers position’ the arms must not be abducted more than 70°11 and should be kept anterior to the sagittal plane12 with the scapulae shrugged13 cranially to avoid caudal traction of the shoulder girdle. The elbows and forearms should be slightly flexed and pronated so as to not create a stretching force along the the median and ulnar nerves14,15.
In addition, pressure palsies are well recognised in other anatomic areas: ischium area (sciatic), the lateral knee/fibula neck (CPN) the medial epicondyle (ulnar) and parotid area (facial nerve). For patients who are spending extended times in critical care the addition of padding to protect the local nerve anatomy may be worth considering.
Differentiation between ‘normal’/expected post critical care weakness and PPP can be difficult. In addition, neurologic dysfunction following a period within critical care can have a number of differing causes16. Direct viral neuropathy17 is rare but should be considered in neuropathies which extend to multiple sites and differing anatomic locations. It is known that other Corona viruses have been documented to be neurotrophic and neuropathic17. There is no specific evidence that this is the case with COVID-19, although the symptoms of loss of smell and taste are thought to be mediated by this mechanism18.
Management
It is impossible to eliminate the risk of nerve injury. The incidence of brachial plexus injury related to prone positioning during the COVID-19 pandemic may never be fully known. Cases will arise and many orthopaedic teams will be called to assess such patients and advise on management. The following protocol for assessment and guidelines for referral are suggested (Figure 2).
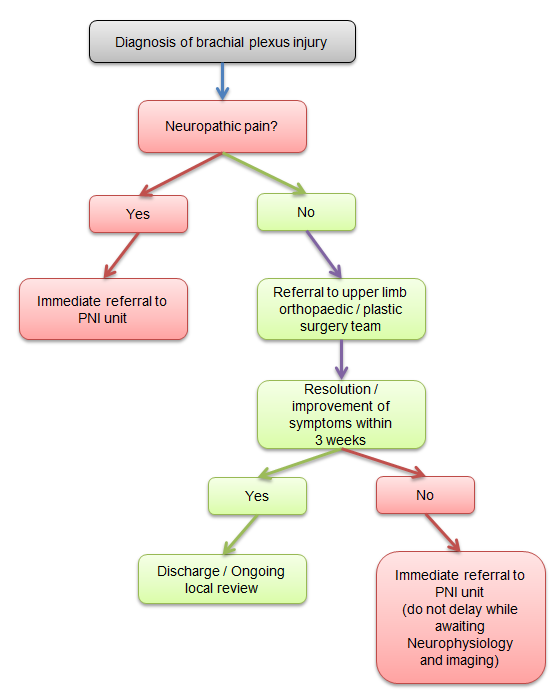
Figure 2. Suggested protocol for assessment and onwards referral for PPP.
Once patients are extubated and gain capacity, it is recommended that a neurologic screening assessment (of the presence of upper limb neuropathic pain, paraesthesia/anaesthesia/dysthesia and motor loss) is performed, (Figure 3). It is likely that those with conduction block (neurapraxia) will resolve spontaneously with no long term issues. Signs that the injury is majority conduction block would be a patchy distribution where sensation and sympathetics are intact, alongside incomplete motor involvement. In this scenario there will be no neuropathic pain. A proportion of patients will have persistent symptoms which do not resolve within 3 weeks. Far from being a benign pathology, compression related nerve injuries, if not treated, have a significant risk of long term morbidity19. It is therefore important that patients who do not recover function within 3 weeks of the symptoms being identified are referred to a centre for nerve injury (Figure 2). Any patients who report the presence of neuropathic pain or a total loss of function of one nerve branch (no sympathetics, sensation or motor) require urgent treatment.
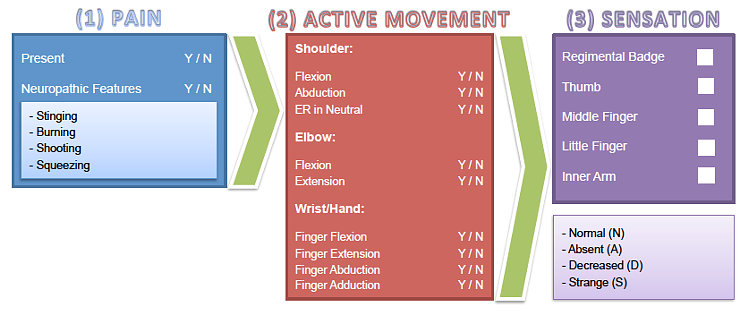
Figure 3. Suggested clinical examination screening tool.
References
- Alderden J, Rondinelli J, Pepper G, Cummins M, Whitney J. Risk factors for pressure injuries among critical care patients: A systematic review. Int J Nurs Stud. 2017;71:97‐114.
- The Faculty of Intensive Care Medicine (2019). Guidance for: Prone Positioning in Adult Critical Care. Available at: https://www.ficm.ac.uk/sites/default/files/prone_position_in_adult_critical_care_2019.pdf.
- Defence Health Agency - Department of Defence (2020). Matos RI, Chung KK. DoD COVID-19 Practice Management Guide. Clinical Management of COVID-19. Available at: http://www.med.umich.edu/surgery/mcccn/documents/DoD-COVID-19-Practice-Management-Guide-V10.
- Bein T, Bischoff M, Brückner U, Gebhardt K, Henzler D, Hermes C. S2e guideline: positioning and early mobilisation in prophylaxis or therapy of pulmonary disorders: Revision 2015: S2e guideline of the German Society of Anaesthesiology and Intensive Care Medicine (DGAI). Anaesthesist. 2015;64 Suppl 1:1-26.
- Oliveira VM, Weschenfelder ME, Deponti G, Condessa R, Loss SH, Bairros PM. Good practices for prone positioning at the bedside: Construction of a care protocol. Rev Assoc Med Bras (1992). 2016;62(3):287-93.
- Association of Surgical Technologists 2011 guidelines AST 2011. Available at: https://www.ast.org/uploadedFiles/Main_Site/Content/About_Us/Standard%20Surgical%20Positioning.pdf.
- Royal National Orthoapaedic Hospital NHS Trust (2020). Prone Positioning Plexopathy: Advice to minimise risk of Brachial Plexus injury. Available at: https://www.rnoh.nhs.uk/application/files/6715/8834/4124/Proning_advice_and_pathway_for_COVID19_patients.pdf.
- Schwartz DM, Sestokas AK, Hilibrand AS, Vaccaro AR, Bose B, Li M, Albert TJ. Neurophysiological identification of position-induced neurologic injury during anterior cervical spine surgery. J Clin Monit Comput. 2006;20(6):437-44.
- Bogduk N, Mercer S. Biomechanics of the cervical spine. I: Normal kinematics. Clin Biomech (Bristol, Avon). 2000;15(9):633-48.
- Mihara A, Kanchiku T, Nishida N, Tagawa H, Ohgi J, Suzuki H. Biomechanical analysis of brachial plexus injury: Availability of three-dimensional finite element model of the brachial plexus. Exp Ther Med. 2018;15(2):1989-93.
- Kam AW, Lam PH, Haen PSWA, Tan M, Shamsudin A, Murrell GAC.Preventing brachial plexus injury during shoulder surgery: a real-time cadaveric study. J Shoulder Elbow Surg. 2018;27(5):912-22.
- Jackson L, Keats AS. Mechanisms of brachial plexus palsy following anaesthesia. Anesthesiology. 1965;26:190-4.
- Kleinrensink GJ, Stoeckart R, Mulder PG, Hoek G, Broek T, Vleeming A, Snijders CJ. Upper limb tension tests as tools in the diagnosis of nerve and plexus lesions. Anatomical and biomechanical aspects. Clin Biomech (Bristol, Avon). 2000;15(1):9-14.
- Nee RJ, Yang CH, Liang CC, Tseng GF, Coppieters MW. Impact of order of movement on nerve strain and longitudinal excursion: a biomechanical study with implications for neurodynamic test sequencing. Man Ther. 2010 Aug;15(4):376-81.
- Dilley A, Lynn B, Greening J, DeLeon N.Quantitative in vivo studies of median nerve sliding in response to wrist, elbow, shoulder and neck movements. Clin Biomech (Bristol, Avon). 2003;18(10):899-907.
- Shepherd S, Batra A, Lerner DP. Review of Critical Illness Myopathy and Neuropathy. Neurohospitalist. 2017;7(1):41-8.
- Hwang CS. Olfactory neuropathy in severe acute respiratory syndrome: Report of a case. Acta Neurol Taiwan. 2006;15(1):26-8.
- Conde Cardona G, Quintana Pájaro LD, Quintero Marzola ID, Ramos Villegas Y, Moscote Salazar LR. Neurotropism of SARS-CoV 2: Mechanisms and manifestations. J Neurol Sci. 2020;412:116824.
- Warner MA, Warner ME, Martin JT. Ulnar Neuropathy: Incidence, Outcome, and Risk Factors in Sedated or Anesthetized Patients. Anesthesiology 1994;81(6):1332-40.
