Best of the Best
The Best Regional Orthopaedics Papers
Training Program Directors across the UK submit the best paper from their region to be presented at the BOA Annual Congress.
The Selection
The 'Best of the Best' candidates are selected every year from each region as the best paper/piece of original research.
Each paper is usually selected at Annual Deanery T&O Research Days round the country, where papers are marked by local consultants and invited judges. Therefore, it really is the best of the best!
The research is limited to trainees' research done in 'normal' training time and not done during OOPR. The research topics can be very diverse but must be related in some way to T&O.
The trainee must be a T&O ST3-8 and be available to present their research in person at the BOA Annual Congress.
The Annual Congress
With all the award-winning papers of each UK Deanery and the Military Deanery, in one place, your esnsured a really exciting and high-quality Best of the Best Session.
The marking is done by the TPDs present at Congress and the winner is awarded the prize during the Awards and Medal ceremony at the Annual Congress.
To win the overall best of the best paper is a tremendous accolade. The winner will get to represent the BOA and present the best abstract at the 26th EFORT Congress 2025.
View the 2024 Best of the Best Nominations below
Birmingham
Exploring the Long-Term Efficacy of Modified Dunn Osteotomy for Severe SCFE: The Birmingham Experience
Authors: Balakumar B, Marson B, Bache CE, Birmingham Childrens Hospital
Abstract:
The Modified Dunn osteotomy is a technique used to manage severe slipped capital femoral epiphysis in children. It helps reduce slips and prevent future complications. The Birmingham experience with this technique is being evaluated in this study to determine its efficacy.
We analysed the outcomes of 57 Modified Dunn osteotomy procedures performed on 56 children by the senior author between 2006 and 2019. In April 2024, we reviewed case notes to determine arthroplasty-free survival rates, avascular necrosis rates, and other complications requiring return to theatre.
The average age at time of slip was 13.5 (SD 1.5) years. The median time to case notes review was 7.6 [IQR 10.3-13.1] years. The 5- and 10-year arthroplasty-free survival was 98.2 (95% CI 99.8-88.0%) and 94.9% (95% CI 98.8-80.2%) respectively. During follow-up, two patients got hip replacements. One for AVN and the other for cartilage damage.
Seven patients were diagnosed with avascular necrosis during the 2-year clinical review, resulting in a 12.3% incidence rate of AVN. Two patients had labral tears, and two cases required additional surgery due to postoperative instability. Out of the 32 children without a simultaneous contralateral pin, 5 (15.6%) developed a contralateral SUFE treated with a pin in situ. Modified Dunn osteotomy offers reliable hip preservation outcomes. 15% contralateral slip risk in children.
Defence Deanery
Ten Years of Direct Skeletal Fixation for Military Veterans; An Overview of Outcomes
Authors: Handford, C. Toderita, D. Hindle, P. Kendrew, J. Evriviades, D. Ramasamy, A. Fenton, P. Foong, D. Bull, AJ, McMenemy, L. The UK Osseointegration Group.
Abstract:
Advancements in trauma care on Operations in Iraq and Afghanistan led to 'unexpected survivors,' primarily highly motivated above-knee amputees unable to mobilise with standard prosthetics due to complex soft tissue injuries. Using LIBOR funding, 21 veterans (35 femoral residuum’s) received OGAP-OPL Direct Skeletal Fixation.
Results from two patient cohorts, the first (13 patients) with surgeries averaging 7.69 (5-10) years and the second (8 patients) treated within the last 2 years following transition to an NHS Consultant led delivery model, indicate promising outcomes.
In the established cohort low explantation rates of 4% (1/23 implants) and minimal chronic suppressive antibiotic use of 15% (2/13 patients) reassure regarding complications due to uncontrolled infection.
The incidence of fractures 11% (4/35 femoral residuum’s) from falls whilst ambulant suggests successful rehabilitation.
Favourable patient-reported outcomes and functional benefits, coupled with cost-effectiveness, advocate for continued research and potential NHS adoption.
East Midlands North
Is Hip Dysplasia Under-reported? A Retrospective Analysis of Pelvic X-rays
Authors: B Oakley, Z Borton, M Sohatee, University Hospitals of Derby and Burton NHS Foundation Trust
Background
Recognition of dysplastic hip morphology is required for timely diagnosis and management of young adult patients presenting with atraumatic hip pain. Hip dysplasia causes pain and the development of premature hip arthritis, its prevalence has been reported to be between 2 and 20% in the general population. This study aims to determine the reporting accuracy of pelvic x rays in adults aged under 40 presenting with hip pain at a single institution.
Methods
140 hips from 70 patients were identified. Patients with traumatic hip pain or x rays requested by an orthopaedic surgeon were excluded from analysis. 132 hips from 64 pelvic X rays were included for final analysis and underwent combined review by the senior author (MS) and a post FRCS SpR (BO) and were categorized into having radiographic signs of dysplasia, borderline dysplasia, impingement or acetabular version abnormalities. The primary radiographic measures of interest were the lateral centre edge angle (LCEA), Tonnis angle and alpha angle. The British Hip Society considers a LCEA of under 25 degrees dysplastic, a Tonnis angle of <0 was categorized as pincer impingement, a Tonnis angle of >10 was considered dysplastic, an alpha angle of >60degrees was considered indicative of impingement. These radiographic findings were correlated against the original report, a diagnosis was considered missed should their radiographic parameters consistent with dysplasia (tonnis >10 or LCEA <25) or impingement (alpha >60 or Tonnis <0) in the context of a “normal” report.
Results
Of the 64 reports, 1 gave a diagnosis of dysplasia, 2 borderline dysplasia and 1 of impingement, 8 diagnosed arthritis and 52 reported no abnormality. 37 (29%) hips had a LCEA of <25degrees, 25 hips (20%) had a tonnis angle of >10 degrees and 10 (8%) had a tonnis angle <0degrees. 37 (29%) had an alpha angle of >60degrees. 36 (28%) had a posterior wall sign, 64 (50%) an ischial spine sign and 48 (38%) a crossover sign. 26 of the 42 (62%) pelvic x rays had radiographic features of dysplasia or impingement that were not reported.
Conclusion
A significant number of patients have radiographic signs of either impingement or dysplasia which are currently being under-reported. Pelvic x rays in patients under 40 with hip pain in the absence of arthritis would benefit from having their LCEA, Tonnis and alpha angles measured routinely to avoid missed diagnosis in the future.
East Midlands South
Novel Technologies for Detecting Relapse in Clubfoot: The Old, The New & The Future.
J. Shepherd, N Horsely, S Wu, D Puttock, P Divall, J Paneerselvam, A Peek
Background
Relapse can occur following initial clubfoot treatment, requiring further intervention. Current practice involves serial examination to monitor for relapse. However, this is resource-intensive and often inaccessible. We therefore aimed to 1) synthesise current evidence to determine whether gait-analysis technology currently available can identify relapse; 2) develop a novel method of recording footprint shape to facilitate future Artificial Intelligence (AI) deep-learning model development to identify relapse.
Methods
Systematic review of the literature was conducted to identify studies comparing gait-analysis in children <18years with clubfoot with and without relapse. End-points included Gait Deviation Index (GDI) and individual kinematic parameters. Random-effects meta-analysis was performed using Stata 17.0 BE. To subsequently develop our novel method, walking-age children with clubfoot were recruited. Water and a patio tile were used to make footprints and images captured with a camera. An AI model automatically processed images to define footprint shape.
Results
Seven studies (306 participants, 343 feet) were included. Reduced dorsiflexion and increased forefoot adduction and supination were observed in relapse. Lower GDI scores were observed in relapse (pooled-mean-difference 5.33, 95%CI 2.57–8.09, p<0.001).
Forty participants were recruited with mean age 76 months (+/-33 SD). Participants had bilateral clubfoot in 50% of cases. The AI-model successfully determined foot outline from images.
Conclusions
GDI and kinematic parameters differ in clubfoot relapse. Increased forefoot adduction is associated with relapse according to gait-analysis and pedobarography literature. Our technique represents a simple way to define foot shape and can therefore facilitate development of a deep-learning AI model to identify relapse.
East of England
Which Radiographic Measures Correlate With Outcomes Following Total Knee Arthroplasty?
Authors: T Barker, I Onubogu, I Mcnamara, V Pomeroy, Dept of Orthopaedics, The Norfolk & Norwich University Hospitals
Background
Rotational malalignment of knee replacements is understood to be associated with poor outcomes. The aim of this study was to correlate a variety of commonly used measurements with patient reported outcome measures.
Methods
Retrospective analysis of prospectively collected data from the Capability RCT comparing Journey II BCS and Gen II TKA including 78 participants. Each participant had pre and postoperative radiographs and CT rotational profiles of both limbs within 8 weeks of surgery. They also completed a number of commonly used PROMS at baseline, 1 week, 6-8 weeks, and 6 months, the primary outcome being OKS at 6 months. Radiographic & CT measurement of several commonly used and some novel parameters was undertaken by 2 T&O registrars. Statistical analysis consisted of interclass coefficient for reliability, multiple regression analysis, and students t-test.
Results
Mean oxford knee score improved from 19.7 (SD 5.5) preoperatively to 42.9 (SD 5.2) at 6 months. Measures that involved the tibial tubercle were less reliable, postoperative TT-TG was not reliable enough for inclusion (ICC 0.557). Multiple regression analysis demonstrated many statistically significant correlations between PROMS and outcome measures at various time points, the most frequently implicated measures were femoral axial alignment, co-axial congruity of femoral/tibial components, and femoral component oversizing, although the R2 was <10% in each case. The only measures that correlated significantly with outcomes at 6 months were femoral component oversizing and co-axial congruity of femoral/tibial components, although the mean difference was less than the MCID.
Conclusion
This study confirms that modest improvements in outcome can be achieved with optimally sized and aligned components, although it isn’t clear what role absolute tibial alignment plays, efforts should be made to develop a clinically/statistically reliably measure of tibial component alignment. Component malalignment did not predispose to a poor outcome in this cohort.
Greater Manchester, Lancashire & South Cumbria
Provision of Radiation PPE across North West England’s Trauma Theatres. Is it Adequate?
Authors: H Sevenoaks, L Murphy, DS Johnson, North West Orthopaedic Research Collaborative.
Aim:
To determine if the orthopaedic surgical workforce were adequately protected by radiation personal protective equipment (PPE) available in trauma theatres in NW England.
Methods:
A snapshot audit of radiation PPE provision and orthopaedic surgical workforce demographics was undertaken between January - July 2023 across 11 hospitals in NW England. Size and appropriateness of radiation PPE for surgeon use (i.e. wraparound protection, ≥0.25mm lead weight equivalence) was correlated with size requirements of the workforce using a bespoke audit tool.
Results:
284 gowns/sets of radiation PPE were evaluated, in correlation with the requirements of 417 members of the medically qualified surgical workforce (FY1 - Consultant) across North West England. For 29.4% (n=123) of surgeons in the region, there was not a single appropriately sized wrap-around gown available for them in their trauma theatres, irrespective of other users requirements. Only 31.7% (n=90) of trauma theatre radiation PPE was acceptable for surgeon use.
Regionally, there was no significant difference in access to appropriately sized standard “unisex” PPE between different workforce groups (rotating vs. permanent staff) or between male and female surgeons. No trusts had enhanced female breast protection PPE available.
Conclusions:
Provision of radiation PPE to surgeons in trauma theatres is inadequate in North West England. This project has since been undertaken in Wessex, via their trainee led research collaborative, utilising our tool to reveal similar deficiencies. BOTA are disseminating our tool across regional representatives to facilitate national improvements in this domain. We encourage all surgeons to appraise their current radiation safety measures and PPE provision and where necessary, take steps to improve it.
Kent, Surrey and Sussex
QIP: Local provision of ionising radiation personal protective equipment (PPE) for female orthopaedic surgeons.
Authors: Madeleine Garner, Moneet Gill, Marta Karbowiak, Ankit Desai
Background:
Use of ionising radiation is commonplace in orthopaedic theatres. The ALARA principle is important for surgeons to be familiar with to mitigate risk to the patient, themselves and their colleagues. The operating surgeon and first assistant receive a significantly higher dose of radiation compared to other theatre staff and trainees typically use more fluoroscopy than consultants. Over the last 10yrs, observational studies have demonstrated an increased prevalence in breast cancer in female orthopaedic surgeons compared to case matched urology and plastic surgeons and a simulation study demonstrated radiation exposure to the UOQ of breast tissue was significantly reduced by PPE with axillary supplements, compared to standard gowns. Subsequently, the BOA published advice, specifically regarding appropriate gowns for female orthopods. The aim of this QIP was to highlight the lack of and subsequently improve local PPE provision.
Patients and Methods:
Systematically, all gowns across 4 orthopaedic theatres were reviewed. Each gown was assessed for: style, size, lead equivalent thickness, if broken, level of axillary coverage, if “personal” and associated thyroid collar.
Results:
45 gowns and 13 thyroid shields were found. Compared to BOA recommendations: a range of sizes were available and 97.8% met the minimum thickness. 86.7% were “tabard” style, deemed UNSUITABLE for female orthopods. There were no options with high axillary protection. No female orthopod had a custom fitted gown.
An intervention was made to purchase 2 new gowns, specifically designed for female orthopods. These were “vest and skirt” style with high axillary protection, elasticated back for better conformity and embroidered to ensure exclusive use.
Conclusions:
These new gowns gave current female orthopods adequate protection. Funding constraints, occupational health policy and rotational training meant we were only able to purchase 2 “non-fitted” gowns, compromising an element of protection to allow “best-fit-for-all”. We would advise trainees check there local PPE suitability and that departments replace broken tabard gowns with skirt/vests with high axillary protection, as these can be used universally.
HENW West (Mersey).
Does the NSQIP Risk Assessment Tool Accurately Predict Post-Operative Complications in a UK Population Undergoing Elective Lower Limb Operations? A Single Centre Analysis
James Chapman1,2, Lebur Rohman3, Sally Hargreaves4, Ed Benison4, Hannah Kennedy4, Alasdair Santini1,2
1Lower Limb Arthroplasty Unit, Department of Orthopaedics, Liverpool University Hospitals NHS Foundation Trust, 2Faculty of Health & Life Sciences, University of Liverpool, 3Department of Orthopaedics, Wythenshawe Hospital, Manchester University NHS Foundation Trust, 4Department of Anaesthetics, Liverpool University Hospitals NHS Foundation Trust
Background: The American College of Surgeons’ NSQIP risk assessment tool is used pre-operatively to aide decisions around elective surgery including predicting post-operative complications. Based on American patients, it has not been validated against our local patient population. We assessed whether patients undergoing surgery demonstrated the predicted post-operative risk profile.
Methods: We analysed prospectively collected NSQIP data on 282 consecutive knee and hip arthroplasty, knee arthroscopy and ACL reconstruction procedures over a four month period including ‘patient’ and ‘average’ risk and post-operative complications. NSQIP ‘average risk’ was used as a matched control for each patient. Patient’s own risk was converted into ‘above’ or ‘below’ average for analysis. Median differences were assessed using Wilcoxon Signed Rank test. Accuracy of prediction was assessed and regression analysis used to assess correlation.
Results: Predicted vs average scores showed reasonable correlation (R2 = .658, p<.001), but median differences between percentage risk calculated were different (3.9 vs 3.1, respectively p<.001). 25 patients suffered a total of 36 NSQIP coded complications, with SSI and readmission the most common (n=7). 4 patients required return to theatre. Predicted risk was more likely to be higher than average risk where a patient suffered ≥1 complication (OR 1.64, p<.001 vs OR 0.678, p=.03). The PPV of an ‘above average’ prediction was 17.2% and ‘serious complication’ was 6.06%; NPV of a ‘below average’ outcome was 95.6% and ‘serious complication’ was 99.45%. Surgical site infection was more likely if predicted as “above average” but did not tend to significance (OR 4.308, p=.06, NPV 98.59%).
Costs: None
Conclusion: NSQIP risk assessment is a useful when discussing patient risk, however its complication prediction is poor and be used with caution in the UK setting. Calibration against a local population is required if it is to be used to influence clinical decision making.
Middlesex/UCH
An Artificial Intelligence Based Approach to Musculoskeletal Acute Knee Injury Triage
Authors: James Dalrymple, Dylan Mistry, Ahmed El-Sheikh, Jiri Mocicka, Mr Shehzaad Khan, Royal National Orthopaedic Hospital
Intro
Acute knee injuries and knee pain affect 25% of the adult population at any one given time in the United Kingdom (UK). In 2023, NHS England reported 230,000 of accident and emergency attendances due to acute knee injuries with an average waiting time of 16.5 weeks to see a specialist for diagnosis. We know these injuries are a significant financial and resourceful burden on our healthcare system.
In addition to early and best care, recent studies have also displayed the importance of the early diagnosis and management of knee injuries, particularly with delayed treatment of anterior cruciate ligament injuries being shown to have poorer long term outcomes (1-6).
The current pathways for these injuries through our healthcare systems are cumbersome and can often result in a delayed diagnosis and/or treatment.
There has been a huge drive and investment in artificial intelligence (AI) over the last decade. It is estimated that AI could cut annual USA healthcare costs by $150 billion by 2026. A considerable component of the cost reduction stems from adopting a proactive health management approach, expected to result in fewer hospitalisations, fewer doctor visits, and reduced treatments.
Our aim is to present a proof of concept study to assess if using AI technology to triage acute knee injuries can correctly identify patients with knee injuries who require Magnetic Resonance Imaging (MRI) prior to specialist review, ultimately streamlining the triage process.
Methods
A retrospective review was performed of patients in a single centre who had attended an acute knee clinic (AKC) and been reviewed by a senior orthopaedic surgeon. A 17 point questionnaire was designed and inputted in to an algorithm using rule-based expert system AI. This emulates the decision-making ability of a human expert, which in our case, is a consultant knee surgeon. All questions were written in a format that a lay person would be able to answer without the need of a medical examination. Answers were multiple choice or binary options. The symptoms and signs from the clinic letters were inputted in to the AI algorithm questionnaire to produce a result if the patient required an MRI scan and a provisional diagnosis. Primary outcome measure was correct identification of patients by algorithm who needed an MRI scan. Secondary outcome was the ability to make the correct diagnosis.
Results
Fifty three patients were included (30 male, 23 female); average age 29.1 (16-39). Mechanisms of injury included 28 from sport, 9 from activities of daily living, 5 from high energy and 11 from low energy. Fifty two patients went on to have an MRI scan performed as a result of the AKC consultation. Injury diagnosis from the AKC consultation were 28 ligament, 13 menisci, 2 minor fracture (osteochondral), 1 normal, 4 patellofemoral and 4 pending results. Our algorithm correctly identified 91% of patients (48) who needed a scan and identified the correct diagnosis in 81% of patients (43). Nineteen patients had dual diagnosis (i.e. ligament and menisci injury) and the AI algorithm was able to correctly identify both diagnosis in 63% of patients (12). Two patients (3.7%) were not recommended a scan from the algorithm. Further analysis showed that both patients had undisplaced posterior horn medial meniscal tears in an age group which would not routinely require initial surgical treatment. One patient (1.9%) did not have a scan, which the algorithm recommended that had a clinical diagnosis of a posterior cruciate and medial collateral ligament injury.
Discussion and Conclusion
This proof of concept study has shown that an AI based algorithm can correctly identify patients with acute knee injuries presenting to primary/secondary care that require MRI imaging with a very high sensitivity and low specificity. This could improve the efficiency and cost effectiveness of the normal patient pathway for these injuries. Ultimately resulting in quicker diagnosis and treatment of these injuries.
Despite this, our study is limited by it’s small sample size. AI technology requires thousands of data inputs in order to prove its reliability and in particular its external validity. There are also the cost implications of introducing such a system alongside the importance of maintaining patient confidentiality while utilising “big data”.
We have shown a proof of concept in using an AI based machine learning algorithm to identify patients with acute knee injuries who require an MRI. This could be used to streamline current patient pathways to reduce cost, improve patient experience and ultimately improve patient outcomes. There is however significant hurdles to overcome prior to mainstream adoption of this technology.
Northern
Association Between Preoperative Glycaemic Control (HbA1c) and Early Outcomes Following Primary Hip and Knee Replacement
Authors: Richard James Holleyman, Michael Clarkson, Amy Shenfine, Kate Martin, James Prentice, Mark Bowditch, Gerry Rayman, Andy Judge & Mike Reed, Northumbria Healthcare & Newcastle University
Background
This study investigates the relationship between Diabetes mellitus (DM), glycated haemoglobin (HbA1c) and postoperative outcomes among patients receiving hip and knee replacement.
Methods
We conducted a single-centre cohort study of patients receiving primary joint replacement between 2008-2019 in whom preoperative HbA1c was recorded. Cases were categorised by preoperative HbA1c as ‘diabetes’ (≥48mmol/mol), ‘prediabetes’ (≥42mmol/mol and <48mmol/mol), ‘no diabetes’ (<42mmol/mol), or in ‘remission’ (preoperative HbA1c <42mmol/mol but having a historic HbA1c result ≥42mmol/mol). Multivariable logistic regression and restricted cubic splines were used to examine the association between diabetes status, HbA1c and early postoperative outcomes.
Results
Analysis of 9,454 cases (18.4% diabetes, 23.5% prediabetes, 49.7% no diabetes, 8.4% in remission) revealed DM was associated with a 50% greater likelihood of experiencing one or more postoperative complications (Odds Ratio (OR) 1.47 (95%CI 1.26-1.71)), a 60% greater risk of acute kidney injury or electrolyte abnormality (OR 1.57 (95%CI 1.33-1.87)), and more than doubling of the risk of postoperative urinary tract infection (OR 2.25 (95%CI 1.15-4.52)) and deep surgical site infection (OR 2.03 (95%CI 1.05-3.86)) compared to patients without diabetes. There was a substantial increase in complication risk as HbA1c entered prediabetes range with no evidence of a plateau or threshold effect, and a profound reduction in the risk of almost all recorded complications for patients in remission from previously elevated HbA1c.
Conclusion
DM was associated with an increased risk of almost all measured early postoperative complications. Interventions to reduce elevated HbA1c, to any degree, may benefit patient outcomes however must be balanced with the risk of iatrogenic harm.
Northern Ireland
A Comparison of Revision Rates for Cementless versus Cemented Fixation for a Single Prosthesis Posterior-stabilised Total Knee Arthroplasty; Medium-term Follow-up of 18,824 cases from the UK National Joint Registry
Authors: Patrick Hickland, Roslyn Cassidy, Owen Diamond, Richard Napier, Outcomes Unit, Primary Joint Unit, Musgrave Park Hospital, Belfast, Northern Ireland
Background
Cementless total knee arthroplasty (TKA) offers a number of conceptual benefits over cemented TKA, and evidence of equivalence exists for certain implant designs. However, the effect of the cam-post interaction of posterior-stabilised (PS)-TKA on implant osseointegration remains uncertain. This study aims to assess the survivorship of cemented and cementless options of a single prosthesis PS-TKA.
Methods
We obtained data from the United Kingdom National Joint Registry (NJR), on patients undergoing primary PS-TKA for osteoarthritis using the Stryker Triathlon system between 1st January 2010 and 31st December 2019. We excluded patients with an implausible body mass index (BMI, <10 or >60 kg/m2), or where there was use of bone graft, revision implants or a hybrid approach to cementation. Statistical analysis was performed using Stata.
Results
There were 18,824 relevant PS-TKA, 1,068 (5.7%) cementless and 17,756 (94.3%) cemented. Those in the former cohort were more likely to be male (48.7% vs 41.9%, p<0.01), of lower median age (70 vs 71 years, p=0.01), higher median BMI (31 vs 30 kg/m2, p<0.01), and shorter median duration of exposure to risk of revision (5.5 vs 6.9 years, p<0.01). Rates of revision did not differ between the cementless and cemented groups, both all-cause (2.4% vs 2.8%, p=0.49), and for aseptic loosening (0.4% vs 0.6%, p=0.29).
Conclusion(s)
Analysis of this data from the UK NJR demonstrates that in the medium-term, there are equivalent rates of revision after cementless and cemented fixation of PS-TKA. Future work should include studies that are prospective in nature and with long-term follow-up.
Implications
To our knowledge, this is the largest study to address our research question, suggesting that either approach to fixation is reasonable for PS-TKA. It complements existing NJR analyses by making a comparison not readily available, for what is currently the most used TKA system in the UK.
Northern Yorkshire
The impact of ethnicity on care and outcome after hip fracture in England and Wales: A population-based study
Sohail Nisar, Leeds Teaching Hospitals NHS Trust
Aims
To determine if patient ethnicity among patients with a hip fracture influences the type of fracture, surgical care, and outcome.
Methods
Observational cohort study using a linked data set combining data from the National Hip Fracture Database and Hospital Episode Statistics in England and Wales. Patients’ odds of dying at one year were modelled using logistic regression with adjustment for ethnicity and clinically relevant covariates.
Results
A total of 563,640 patients were included between 1 April 2011 and 1 October 2020. Of these, 476,469 (85%) had a coded ethnicity for analysis. Non-white patients tended to be younger (mean 81.2 vs 83.0 years), and were more commonly male (34.9% vs 28.5%, p < 0.001). They were less likely to be admitted from institutional care (12.9% vs 21.8%, p < 0.001), to have normal cognition (53.3% vs 62.0%, p < 0.001), and to be free of comorbidities (22.0% vs 26.8%, p < 0.001), but were more likely to be from the most deprived areas (29.4% vs 17.3%, p < 0.001). Non-white patients were more likely to experience delay to surgery for medical reasons (14.8% vs 12.7%, p < 0.001), more likely to be treated with an intramedullary nail or a sliding hip screw (52.5% vs 45.1%, p < 0.001), and less likely to be mobilized by the day after surgery (74.3% vs 79,0%, p < 0.001). Mortality was higher among non-white inpatients (9.2% vs 8.4% for white), but was lower at one year after hip fracture (26.6% vs 30.3%).
Conclusion
Our study identified serious problems with the quality of NHS ethnicity data. Despite this, we have shown that there is complex variation in case-mix and hip fracture morphology between ethnic groups. We have also identified variations in care received between ethnic groups, and that disparities in healthcare may contribute to poorer outcome. Inpatient mortality is higher in non-white patients, although this finding reverses after discharge, and one-year mortality is lower. Patients from ethnic minority backgrounds experience disparities in healthcare, however at one-year postoperative non-white patients have a statistically significant lower mortality after controlling for relevant clinical covariates.
Oswestry
Non-Selective Enhanced Recovery after Total Hip and Knee Arthroplasty: Experience of 1364 Consecutive Cases in a High-Volume Tertiary Centre
Authors: Menon D1,2, Warren R1, E Dickenson1, Redfern D1, Graham N1, Thomas G1,2
- The Robert Jones and Agnes Hunt Orthopaedic Hospital NHS Foundation Trust, Oswestry, Shropshire, SY10 7AG
- School of Medicine, Keele University, Staffordshire, ST5 5BG
Introduction
Enhanced Recovery after Surgery (ERAS) in total joint arthroplasty improves clinical outcomes and patient satisfaction. However, current evidence is frequently based on its use in a selected healthy population with low patient numbers. This study reports outcomes of ERAS in patients undergoing lower limb arthroplasty not selected on co-morbidity status or age.
Methods
A standardised ERAS pathway was developed. Key themes included: 1. Pre-operative patient education via the ‘Joint School’ service 2. Nutritional status optimisation with high-energy drinks pre- and post-operatively 3. Standardisation of peri-operative analgesia 4. Early physiotherapy promoting post-operative mobilisation 5. Early telephone follow-up following discharge. 1364 patients undergoing ERAS following primary total hip (THA), total knee (TKA) and unicompartmental knee arthroplasty (UKA) between March 2023 and January 2024 were included. Outcomes included short-term (30-day) re-admission rate and length of stay.
Results
Individuals ranged from 19 to 96 years, with mean age 67.9 (SD: 10.6) years and mean ASA 2.1 (SD: 0.6). 91.8% cases followed the peri-operative anaesthetic protocol, and 42.5% attended Joint School pre-operatively. Mode post-operative day of mobilisation was 0 (day 0: 68.0%, day 1: 31.7%).
Similar short-term re-admission rates with significant reductions in mean LOS were noted when compared to 1076 primary THA/TKA performed between October 2022 and March 2023 6-months prior to ERAS pathway introduction (LOS: 1.9 [2.6] vs 3.9 [4.6] days, p<0.001; 30-day re-admissions: 1.4% vs 1.3%, p=0.99). Difference in mean LOS between ERAS and non-ERAS groups was greatest in individuals aged >80 years (≤60 years: 1.4 vs 3.0; 61-70 years: 1.6 vs 3.5; 71-80 years: 2.3 vs 4.0; >80 years: 3.0 vs 6.8). Individuals attending Joint School had lower mean LOS versus non-attenders (1.8 vs 2.9 days).
Discussion
This standardised ERAS protocol is safe and effective, demonstrating high early post-operative mobilisation rates and low 30-day re-admission rates. Reduced LOS associated with ERAS, due to early recovery and return to function, has enormous potential to increase bed capacity in a cost-effective manner. Pre-operative patient education appears a key driver in improving outcomes. Reduction in morbidity appear most marked in individuals of increasing age and co-morbid status, and individuals should therefore not be selected for based on these factors.
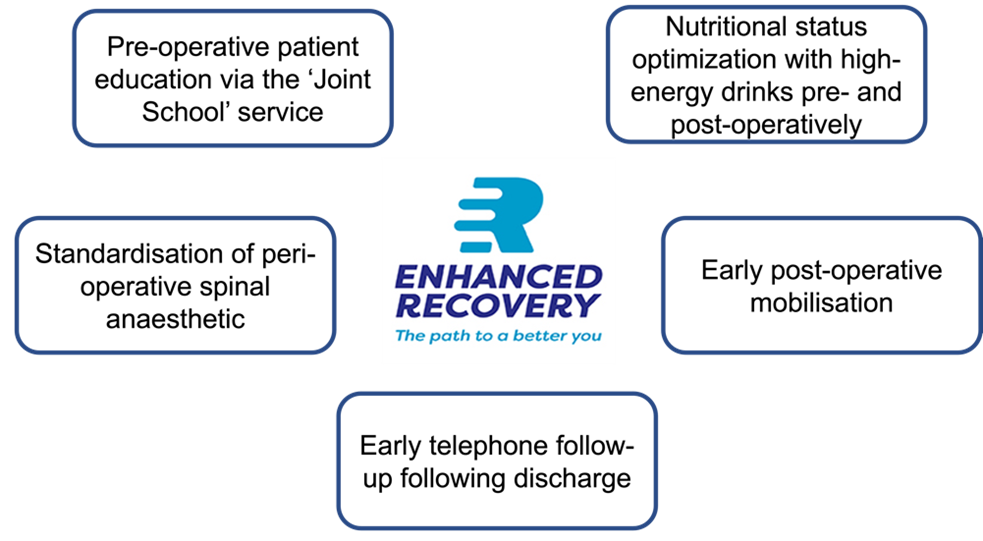
Figure 1 – Components of the ERAS Pathway
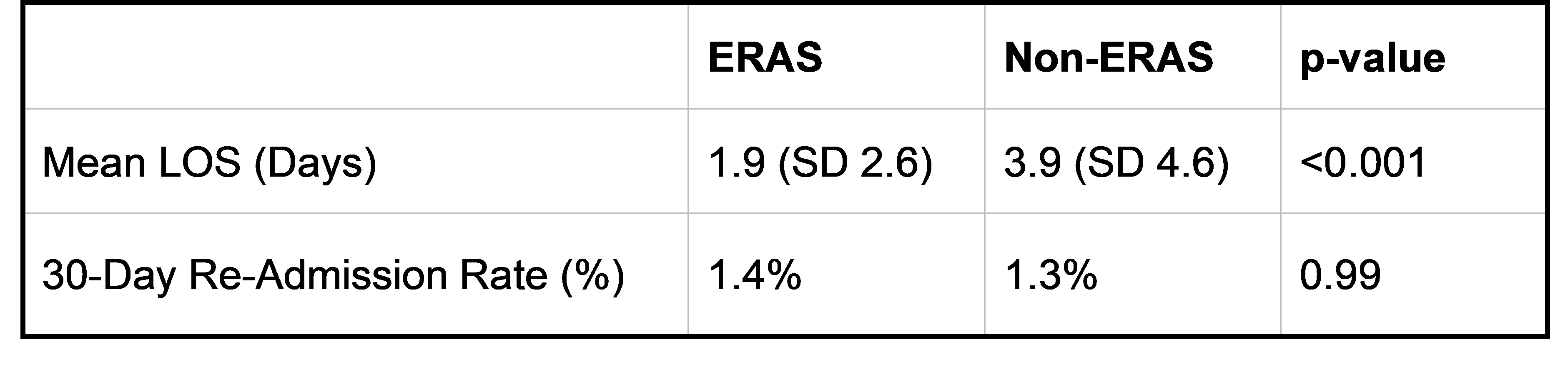
Table 1- Comparison of LOS and 30-day re-admission rates between ERAS and Non-ERAS Cohorts
Oxford
WARP: Results Of The Wycombe Arthroplasty Rapid-Recovery Pathway
Authors: John McNamara, Jane Eastman, Sakis Pollalis, Aniko Frigyik, Royal Berkshire Hospital
Background
Enhanced recovery after surgery (ERAS) protocols produce significant clinical and economic benefits in a range of surgical subspecialties. The development and implementation of such programmes are a growing area of interest in orthopaedics. Rapid recovery programmes offer a multimodal approach directed towards systemic modulation of the surgical stress response to enhance patient outcomes.
Objectives
The Wycombe Arthroplasty Rapid-Recovery Pathway was designed to streamline hip and knee joint arthroplasty to reduce time spent in hospital whilst optimising outcomes in an NHS District General Hospital. The pathway has been designed to manage patient expectations, maximise efficiency, reduce anaesthetic and surgical stress to the patient, optimise pain management and ensure timely therapy input and follow up post-discharge.
Study Design & Methods
1218 patients were admitted acorss a 2 year period to Wycombe General Hospital for elective joint replacement. 378 (31%) of pateints were admitted under the WARP pathway, 839 (69%) were admitted on the standard pathway. Baseline characteristics were similar for both cohorts. Data was collected on operation type, anaesthetic choice, physiotherpy sessions, time of mobilisation, length of stay and inpatient morbidity data.
Results
378 (31%) patients were admitted under the WARP pathway with an average length of stay of 2.2 days with 3.5 physio sessions, 60% had no day two morbidity, 11% were discharged as a day case. 43% mobilised on day 0. 839 (69%) pateints were concurrently admitted on the standard pathway, average length of stay was 3.6 days with 4.2 physio sessions, 49% had no day two morbidity. 0% were discharged on the day of surgery. 12% mobilised on day 0.
Conclusions
Our cohort study shows that the initiation of a Rapid Recovery pathway for joint arthroplasty decreases length of stay, decreases the time to first mobilisation, and decreases inpatient morbidity from joint arthroplasty in an NHS District General Hospital
Republic of Ireland
The Current Standard of the Shoulder Trauma Series in Ireland – A National Audit
Authors: Rosie Mc Colgana,*, Aoife S. O'Halloranb , Patrick J. Carrolla , Ken Kaarc , Kieran O'Sheaa
a St. Vincent's University Hospital, Elm Park, Dublin 4, D04 T6F4, Ireland, b Connolly Hospital Blanchardstown, Mill Road, Blanchardstown, Dublin, D15 X40D, Ireland, c University Hospital Galway, Newcastle Road, Galway, H91 YR71, Ireland
Objectives/aims
The primary aim of this study was to assess the current standard of shoulder radiographs in Ireland. The secondary aim of this study was to determine whether orthopaedic surgeons in Ireland are of the
opinion that a national protocol is required, and what this protocol should consist of.
Methods
A national audit of shoulder trauma series x-rays performed in emergency departments was conducted. The number and type of views performed was recorded. The anteroposterior (AP) and axillary or Velpeau views were assessed to determine if they met pre-defined audit criteria. Consultant orthopaedic surgeons working in public trauma hospitals were invited to participate in an online survey by email.
Results
The number of shoulder trauma series included in this audit was 789. The majority of patients had two views performed (75.92%, n ¼ 599) and 21.17% (n ¼ 167) had an axillary or Velpeau view. The AP view met the audit criteria in 23.09% (n ¼ 181) of cases. The survey response rate was 70.8% (n ¼ 17). 88.2% (n ¼ 15) of surgeons agreed that three views should be performed for a shoulder trauma series and 94.12% (n ¼ 16) agreed that an axillary or Velpeau view should be included. The majority of surgeons surveyed (94%, n ¼ 16) are in favour of establishing a national protocol.
Conclusion
The current standard shoulder trauma series in Irish hospitals consists of two views, most frequently a thoracic AP and a scapular Y view. We propose the introduction of a national protocol consisting of three views: Grashey AP, Scapular Y, and an axillary or Velpeau view.
Royal London
Calcaneum Fracture Management - An Experience from a Large Major Trauma Centre
Authors - B Gabbott, I Drummond, M. Dewhurst, T Walker, S Shah, A Patel, L Parker, F Malagalada, L Jeyaseelan
Background
Calcaneum fractures are high energy, complex injuries, providing anatomical and technical treatment challenges. There is a ongoing debate as to their best management, with high complication rate and potentially poor outcomes. The aim of our study was to analyse the outcomes of these injuries from a large trauma centre series, and identify which patients are at highest risk.
Method
Retrospective data collection from a a single high volume major trauma centre, between 2017 – 2021. Included patients must be 18+ years old with minimum 3 months follow. Retrospective review of case notes and imaging was conducted to collate demographic data, fracture classification and treatment. Outcomes of interest were complications, further surgery and arthritis. Subgroup analysis on sanders classification, smokers and open injuries. Regressional modelling statistics used to analyse risk factor association with outcomes.
Results
170 cases identified, mean age 50 with male predominance (74%). 97(57%) were intra-articular, with sanders 3 most common. 3most prevalent associated fractures include ipsilateral foot, lumbar vertebrae and pelvis. Sanders classification does not associate with operative fixation. Those patients operated on with sanders 3 + 4, smokers and open injuries have complications and revision rates +25%. Smokers and open fractures significantly associated with revision and complication rate using regression modelling.
Conclusion
We present the experiences of a major trauma centres treatment of this complex fracture, and it’s associated morbidity. We show a higher than previously documented incidence of mid and fore foot injury in this patient cohort and advise a full foot CT as part of standard work up. Sanders classification does not correlate with operative fixation, and multiple other factors should be considered before deciding treatment. Patients at high risk (open, smokers) should be appropriately consented that operative management has 25% complication + revision rate.
Scotland East - Dundee
Early Management of Paediatric Forearm Fractures in a Major Trauma Centre: An Audit of BOAST Guidelines
Authors: C. Sreenan, E. Fraser, G. Love, Trauma & Orthopaedic Department, Ninewells Hospital, Dundee
Introduction:
The forearm is the most common site of fracture in the paediatric population. Recently published British Orthopaedic Association Standards for Trauma and Orthopaedics (BOAST) guidance has provided clarity in the management of these injuries. In fractures not requiring surgical intervention, early closed manipulation and casting is a suitable treatment option that avoids operative morbidity, theatre resource and reduces length of stay. The aim of this audit was to assess adherence to this guidance in the East of Scotland.
Methods:
All paediatric patients with forearm fractures were identified from East of Scotland trauma lists from 01/03/2023 to 31/08/2023. Their management was compared to the gold standard BOAST guideline: “Early Management of the Paediatric Forearm Fracture” using their inclusion and exclusion criteria.
Results:
79 patients were identified as having had a forearm fracture(s), of which 29 (37%) were excluded. Of the remaining 50, 41 patients (82%) underwent manipulation and cast application in theatre; the other 9 (18%) were treated without a general anaesthetic. The most common injuries sustained were isolated distal radius fractures (25, 50%) and dual midshaft radius and ulna fractures (13, 26%).
Discussion:
Hospitalisation can be a distressing experience for paediatric patients. Most patients included in this cohort required at least an overnight stay in the paediatric unit and a general anaesthetic. This audit has identified scope for improvement with adherence to national guidance. We propose that a trust pathway for early reduction of these injuries could streamline the hospital route for paediatric patients whilst reducing costs.
Scotland South East - Edinburgh
Delay to Theatre Due to Limited Theatre Capacity is Associated with an Increased Mortality Risk in Hip Fracture Patients at 1 Year
Authors: KM Phoon, AD Duckworth, ND Clement, Edinburgh Orthopaedics, Royal Infirmary of Edinburgh, Edinburgh
Background
The primary aim of this study was to assess whether delay to theatre (>36 hours from admission) for surgical management of hip fractures due to theatre capacity was independently associated with a higher mortality. The secondary aim was to assess whether time to theatre was associated with an increased length of stay in hospital.
Methods
This was a retrospective study of patients aged ≥50 years admitted with an acute hip fracture to a single, high-volume orthopaedic trauma centre over a 5-year study period (January 2019 to December 2023). Patients were identified from the local hip fracture database and further data obtained from electronic health records. Data collected included patient demographics, time of presentation and discharge from the emergency department (ED) and orthopaedic department, time to theatre, fracture type and management, length of stay, discharge destination, and mortality.
Results
A total of 5551 patients underwent surgical management of hip fractures during this study period, of which 1160 (20.9%) had surgery delayed by >36 hours. Of those that were delayed, 464 patients were delayed due to limited theatre capacity. There was no significant difference in mortality at 30-day (p=0.459) and 60-day (p=0.617) survival. However, there was a significantly increased risk of mortality at 1-year in patients who were delayed, (less than 36 hours 75.4% versus delayed >36 hours 71%). When adjusting for confounding factors between the two groups delayed to theatre was independently associated with a increased mortality risk (hazard ratio of 1.34, 95% CI 1.16 to 1.54, p<0.001). Furthermore, length of stay in hospital was 3 days longer in the delayed group (p<0.001).
Conclusion
Delayed time to surgery of >36 hours due to limited theatre capacity was independently associated with an increased mortality at 1-year and increased length of stay in hospital in patients with an acute hip fracture.
Scotland West - Glasgow
The SU-PERiosteum – Improving Bone Biology using Novel Chimeric Fibulaperiosteal Flap
Authors: Gagori Bandopadhyay1, Steven Lo2, Indira Yonjan2, Anna Rose2, Giles Roditi1, Colin Drury1, Angus Maclean1
1 Glasgow Royal Infirmary, Glasgow, 2 Canniesburn Regional Plastic Surgery and Burns Unit, Glasgow
Introduction:
The presence of pluripotent mesenchymal cells in the periosteum along with the growth factors produced or released following injury provides this tissue with an important role in bone healing. Utilising this property, vascularised periosteal flaps may increase the union rates in recalcitrant atrophic long bone non-union. The novel chimeric fibula-periosteal flap utilises the periosteum raised on an independent periosteal vessel, thus allowing the periosteum to be inset freely around the osteotomy site, improving bone biology.
Patients and methods:
Ten patients, with established non-union, underwent fibula-periosteal chimeric flaps
(2016-2022) at the Canniesburn Plastic Surgery Unit, UK. Preoperative CT angiography was performed to identify the periosteal branches. A case-control approach was used. Patients acted as their own controls, which obviated patient specific risks for non-union. One osteotomy site was covered by the chimeric periosteal flap and one without. In two patients both the osteotomies were covered using a long periosteal flap.
Results:
The mean bone gap was 7.5 cm. A chimeric periosteal flap was used in 12 of the 20 osteotomy sites. Union rate of 100% (11/11) was noted with periosteal flap osteotomies, versus those without flaps at 28.6% (2/7) (p = 0.0025). Time to union was also reduced in the periosteal flaps at 8.5 months versus 16.75 months in the control group (p = 0.023). Survival curves with a hazard ratio of 4.1, equating to a 4 times higher chance of union with periosteal flaps (log-rank p = 0.0016) was observed.
Conclusion:
The chimeric fibula-periosteal flap provides an option for atrophic recalcitrant nonunions where use of vascularised fibula graft alone may not provide an adequate biological environment for consolidation.
Severn
Displaced paediatric forearm fracture management in the emergency department: how can we achieve best practice? A South West inter-specialty survey and force field analysis.
Authors: Robert Whitham1,2, Luke Duggleby1,2, Catherine Carpenter-Clawson2, Tania Sparks2, Guy Atherton2,3
Institutions: 1Royal United Hospital, Bath, 2South West Surgery in Children Operational Delivery Network, 3Bristol Royal Hospital for Children,
Background
A significant proportion of angulated paediatric forearm fractures requiring definitive manipulation and casting can be treated in the emergency department (ED) rather than an operating theatre. The aim of this study was to evaluate attitudes, barriers and enabling factors that contribute towards the delivery of paediatric forearm fracture manipulations in EDs across the South West of England.
Methods
In collaboration with the South West Surgery in Children Operational Delivery Network (SW SIC ODN), a self-administered electronic survey of clinicians working in Trauma and Orthopaedic (T&O) and Emergency Departments was developed using Google Forms. This was distributed through SW SIC ODN and local communication networks. Prominent themes were identified.
Results
Sixty-five responses were evaluated from 11 hospitals; the majority were from registrars (51%) and consultants (37%). Most hospitals have local guidelines for paediatric forearm manipulation (7/11) and procedural sedation (9/11), although 33% of clinicians were unsure whether these existed. For an angulated mid-shaft both-bone forearm fracture, procedural sedation is perceived to be more successful than intranasal fentanyl and nitrous oxide (69%). The most cited barriers to performing forearm manipulations in ED were physical space (69% agree/strongly agree), staff availability (72% agree/strongly agree) and skillset (available doctors trained in procedural sedation). Broad themes established included: clinician autonomy and advocacy for patients, analgesic versus sedative approach, logistics, availability of senior support, fear of failed attempts, and clinical prioritisation out of hours.
Conclusions
Clinicians report frustration to perceived barriers. Departments allude to opposing priorities based upon clinical demands of the systems in which we work. Although procedural sedation is preferred by clinicians, delivery of best practice (especially out of hours) is often limited by logistical barriers that may benefit from flexible pathways and staffing models.
South East London
Single Mobility Thumb CMCJ Replacement: Early Results in a Single Surgeon Cohort
Authors: Ekemini Ekpo, Sameer Gidwani, Guy's and St Thomas' NHS Foundation Trust
Objective:
Thumb carpometacarpal joint (CMCJ) osteoarthritis is a common and debilitating condition affecting 1.5% of the population. Trapeziectomy been considered the gold standard for surgical management. However, CMCJ replacement is also an option, particularly in younger, higher demand patients, as it potentially offers better preservation of pinch strength and a faster recovery.
Study Design and Methods:
A prospective cohort study design was used. All patients who underwent a Maia thumb CMCJ replacement from January 2017 to January 2024 by a single surgeon were included. Data collected included age, sex, pre-operative and post operative Patient Rated Wrist/Hand Evaluation (PRWHE), and pre- and post-operative lateral pinch strength. All complications and subsequent revisions were also recorded.
Results:
There were 35 patients in total. The mean age of patients undergoing CMCJ replacement was 59.3 years. 86% were female and 14 % were male. The mean follow up was 40 months (1-76). The mean pre-operative PRWHE score was 59.3. The mean pre-operative key pinch was 3.5kg. Postoperatively, the mean PRWHE score decreased to 15.6 while the mean key pinch score increased to 6.5kg. Four patients suffered minor complications which resolved with steroid injections.
Conclusion:
Single mobility CMCJ replacement has demonstrated improved function and excellent pain outcomes with a low revision rates in our series. We recommend its use in active patients with minimally affected STT joints. Further studies are required that compare the outcomes of trapeziectomy versus implants, and single versus dual mobility implants, both in terms of complications and longevity.
South West Peninsula
What are the Demographics and Ethnicity of Patients who have THR/TKR at SWLEOC: Do Interventions and Outcomes Vary by Age, Sex, Ethnicity or Social Deprivation?
Author: Olusegun Ayeko, University Hospitals Plymouth
Aims:
The aim of this study is to describe the demographics of patients undergoing hip and knee replacement at The South West London Elective Orthopaedic Centre (SWLEOC) and examine whether they are associated with 1-year Patient Reported Outcome Measures and the change from baseline.
Patients:
SWLEOC patients who underwent primary Total Hip or Knee joint replacement during the whole calendar years 2019 and 2021.
Methods:
A retrospective analysis of prospectively collected data from SWLEOC was obtained electronically. The primary outcome measures were changes in Oxford Hip and Knee Scores, EQ-5D Index and EQ-5D-VAS scores from baseline to 1-year. The secondary outcomes were time on waiting list and length of stay. We calculated associations of age, sex, ethnicity and deprivation with baseline, 1-year and the change in Patient Reported Outcome Measures using multivariable regression.
Results:
There were 2,502 Total Hip Replacements and 2,763 Total Knee Replacements 2411 and 2611 patients respectively. Patients younger than 60 years, female sex, South Asian ethnicity and in the most deprived decile had lower baseline and 1-year Oxford Hip and Knee Scores. Changes in PROM score and waiting list time did not vary between patient demographic and ethnicity groups.
Conclusion:
Age, sex, ethnicity and deprivation are intertwined in health behaviour and outcomes, with negative associations observed. It must be recognised that detrimental biases and risks exist for these groups.
South Yorkshire
Surgical Utilisation of Performance Enhancing Routines: The SUPER Study
J. Murray1,2, E. Howie3,4, R. Clarke5, N. Totton2,6, A. Peckham-Cooper7,8, H. Church9, S. Yule3,4, J. Tomlinson1,2
1 Sheffield Teaching Hospitals, 2 The University of Sheffield, 3 Clinical Surgery, University of Edinburgh & Royal Infirmary of Edinburgh, 4 Edinburgh Surgical Sabermetrics Group, University of Edinburgh, 5 NHS England, 6 Sheffield Centre for Health and Related Research, 7 Leeds Institute of Emergency General Surgery, St James’s University Hospital, 8 University of Leeds, 9 Faculty of Medicine and Health Sciences, University of Nottingham
Introduction
Performance enhancing routines (PER) are commonly taught in professional sport to control emotion and optimise performance. These lessons are applicable in surgery, where expertise relies on the combination of cognitive processes and technical skills. The aim of this study was to evaluate whether teaching PER to trainee surgeons has the potential to reduce cognitive load, and improve surgical performance.
Methods
Inclusion criteria included SHO-level doctors with an interest in surgery. Participants were randomised into a control arm (no PER training) and an intervention arm (PER training). Participants completed a range of supervised laparoscopic tasks, pre and post intervention, on a standardised laparoscopic box trainer. Data was collected on participants’ subjective levels of cognitive load (questionnaires), objective levels of cognitive load (wearable hardware) and surgical performance (video analysis).
Results
In total, 29 participants were randomised (14-control, 15-intervention). Subjective cognitive load improved in both arms of the study. The control arm had a mean improvement of -2.21, compared to a mean improvement in the intervention arm of -4.67 (adjusted difference=-2.15 (95% CI:-7.09,2.80)). Greater improvements in levels of mental fatigue, feelings of time pressure, task complexity, anxiousness and distraction were observed in the intervention arm, compared to control. Objective levels of cognitive load remained constant for both arms.
Surgical performance did not improve in the control arm (mean = -0.3) but did improve in the intervention arm (mean=1.7, adjusted difference=1.91 (95% CI:-2.22,6.04)). The intervention arm had improved depth perception, dexterity, efficiency, tissue handling and autonomy, compared to control.
Statistically significant correlations were seen between measures of subjective cognitive load and overall surgical performance.
Conclusion
Findings from this surgical sabermetric feasibility study show a benefit of PER in controlling subjective cognitive load and improving overall surgical performance.
This study is the first of its kind in the world and will be used to inform larger scale studies.
Stanmore
A comparative study reviewing post-operative bracing and functional outcomes after scoliosis correction surgery
Authors: Sachi Shah, Aman Sharma, Matthieu Durand-Hill, Helen Hartshorn, Julian Leong, Hilali Noordeen, Jan Lehovsky, Alexander Gibson
Introduction
Thoracolumbar sacral orthosis and soft braces are used routinely after spinal deformity correction surgery. Incremental surgical advances with robust stabilisation has changed the post- operative paradigm and allowed for early mobilisation.
Method
This comparative study evaluates the effect of post-operative bracing on patient reported outcomes (PROMS), clinical and radiological outcomes and cost of patient care. The demographic data (age, sex, comorbidities, cobb angle) and patient reported outcome measures were analysed.
Results
117 patients were included from a single tertiary centre (24 male, 93 female, mean age 17.83). In the braced group (N=58), mean Cobb angle at 6 weeks was 17.91 and 17.44 at 6 months (-0.47 loss of correction). In the unbraced group, mean Cobb angle was 24.10 at 6 weeks and 24.03 at 6 months (-0.07 loss of correction). The difference in loss of correction between both groups was not statistically significant (two-tailed p value = 0.285). The unbraced cohort had better mental health PROMS scores which was statistically significant at 6 months and 1 year (p= 0.036 and p=0.039 respectively). There was no statistically significant difference in both groups when comparing function, pain, self-image and satisfaction scores. Brace use has significant cost implications (£360/brace) as well as increasing length of stay (£368/day).
Conclusion
This is the first patient reported outcome study evaluating post-operative brace versus no brace in spinal deformity correction surgery with no statistical difference in clinical and functional outcomes
Wales
Radiation PPE and Surgical Performance; a Study Using a Simulated DHS Model
Authors: Francesca Solari1, Emma Barlow1, R J Egan1, Wyn G Lewis2, Clare Carpenter2
1Department of Surgery, Morriston Hospital, Swansea, 2 University Hospital of Wales, Cardiff
Contributing authors: Beibit Bashabayev, Kanwalnaini Cheema, Martin Clarkson, Joanna Craven, Kumar Dash, Zayd Jawad, Claire Joyner, Charles Kimberley, Daniel Lewandowski, Clara Miller, Deepika Pinto, Lilly Ryan-Harper, Chris Woodward and Tariq Yasin
Introduction
Radiation Personal Protective Equipment (RPPE) is the subject of safety guidance from the British Orthopaedic Association (BOA). This study aimed to examine potential performance differences in Trauma and Orthopaedic (T&O) Higher Surgical Trainees (HST) undertaking simulated Dynamic Hip Screw (DHS) surgery related to different RPPE attire.
Methods
Fourteen volunteers (8 male, 6 female HSTs) performed two simulated DHS procedures wearing two RPPE attire styles; One Piece (OP) tabard, and Two-Piece skirt/top (TP) both 0.35mm thickness, with a 0.5mm thyroid guard. Continuous Heart Rate (HR) monitoring, temperature, and Visual Analogue Scales (VAS) for comfort and fatigue were measured before and after simulations.
Results
Mean (SD) HR in OP and TP were: HR OP 98.8 bpm (10.3) vs. TP 98.1 bpm (10.8, p <0.001), Maximum HR OP 115.1 bpm (SD 12.4) vs. TP 113.4 bpm (SD 11.9) (p <0.001). Mean change in temperature were OP 0oc and TP -0.03oc (p <0.001). Mean temperature VAS scores in OP were 1.9 (1.7) vs. TP 2.0 (1.4, p <0.001). Comfort VAS scores were: OP 3.1 (2.4) vs. TP 1.7 (2.1, p <0.001) and Fatigue OP 1.4 (1.9) vs. TP 0.8 (1.5, p <0.12).
Discussion
Important differences in surgeon physiological measures (HR, temperature) and self-reported measures of comfort and temperature were found related to RPPE style. Understanding the effects that specific RPPE options have on performance should influence decisions on RPPE choice.
Warwick
Tönnis Angle and Acetabular Depth Ratio: Predictors of Dislocation Following Hemiarthroplasty for Hip Fracture
Authors: Vatsal Gupta, Mohamed Yassin, Darryl Ramoutar, Thomas Hunter
Background:
Despite efforts to mitigate possible modifiable risk factors, dislocations following hemiarthroplasty for hip fracture still occur, with reported incidence rates ranging from 1.5 to 11%. The aim of this study was to investigate whether acetabular dysplasia is a significant contributing factor to dislocation, and since non-modifiable, whether it should affect patient selection for this treatment option.
Methods:
This is a multicentre nested case-control study of patients treated at 2 separate centres over a 10-year period from January 2011 to December 2020. All cases of hemiarthroplasty dislocation following hip fracture were identified from local databases, and 4 random controls were selected for every case. Tönnis angle (TA) and Acetabular-depth-ratio (ADR) was measured on the injured side using AP pelvis radiographs. Patients with TA > 10° and/or ADR < 250 were considered to have abnormal acetabular morphology.
Results:
35 cases of dislocation were identified and 140 random controls were selected. Cases of dislocation had a larger mean TA (8.8° vs. 5.5°, p < 0.001) and lower mean ADR (254 vs. 289, p < 0.001) than controls. 20 out of 35 (57%) cases were considered to have abnormal acetabular morphology, compared to 19 out of 140 (14%) controls. The odds of dislocation is 8.5 times greater (odds ratio = 8.49, 95%CI = 3.73, 19.39) in patients with abnormal TA and/or ADR.
Conclusions:
This study demonstrates that TA > 10° and ADR < 250 are useful criteria to identify patients at greater risk of hip hemiarthroplasty dislocation due to acetabular dysplasia. Special consideration to preoperative planning should be taken in these patients. Future research should focus on methods to minimise risk in this subset of patients, including evaluating total hip arthroplasty with dual mobility component vs hemiarthroplasty.
Wessex
Hyponatraemia in Lower Limb Arthroplasty Increases Length of Stay but Reliably Corrects on Follow-up Bloods. Can we Safely Discharge Patients Earlier?
Authors: Alexander Denning, Rabia Iqbal, Julia Craggs, Ffion Byrn, Toby Briant-Evans
Introduction
Postoperative hyponatraemia is common in elective orthopaedics, however patient management guidelines are lacking. Literature on hyponatraemia’s effect on length of stay (LOS) is limited and there is paucity of data on follow-up bloods. We analysed LOS and follow-up bloods aiming to identify trends which may aid our discharge decisions in elective orthopaedic patients with hyponatraemia.
Methods
We performed retrospective data collection over 6 months in 2023 at 2 hospitals performing lower limb arthroplasty. We collated the patient demographics, pre, post-operative and follow-up sodium levels performed following discharge.
Results
We included 456 patients. 214 had TKR, 203 had THR and 39 had UKR. 25% patients had postoperative hyponatraemia, of those 70% were mild, 26% were moderate, 4% were severe. The groups were matched for mean age (hyponatraemia 70, normal 69) and mean ASA (hyponatraemia 2.8, normal 2.6). Our data showed the LOS for hyponatraemic patients was 3.6 days compared to 2.3 in those with normal postoperative sodium. 25% of hyponatraemic patients had follow-up outpatient bloods, 95% showed an increase in sodium, with an average increase of 4.5mmoL. 90% returned back to their baseline hyponatraemia level.
Conclusion
We demonstrate that LOS in patients with postoperative hyponatraemia is over a 1 day more than patients with normal postoperative sodium. We also demonstrated a reliable correction in sodium levels once discharged. We feel we can use this data to implement guidelines to discharge patients with postoperative hyponatraemia sooner, taking strain off the service and allowing patients to return to their home comforts earlier.
For further details on the Best of the Best Session, please do not hesitate to contact the BOA Events Team via [email protected]
