Programme 2021
Return to Congress HomepageBOA Annual Congress ticket holders are able to watch session recordings after 24 hours of the sessions taking place, which are accessible here.
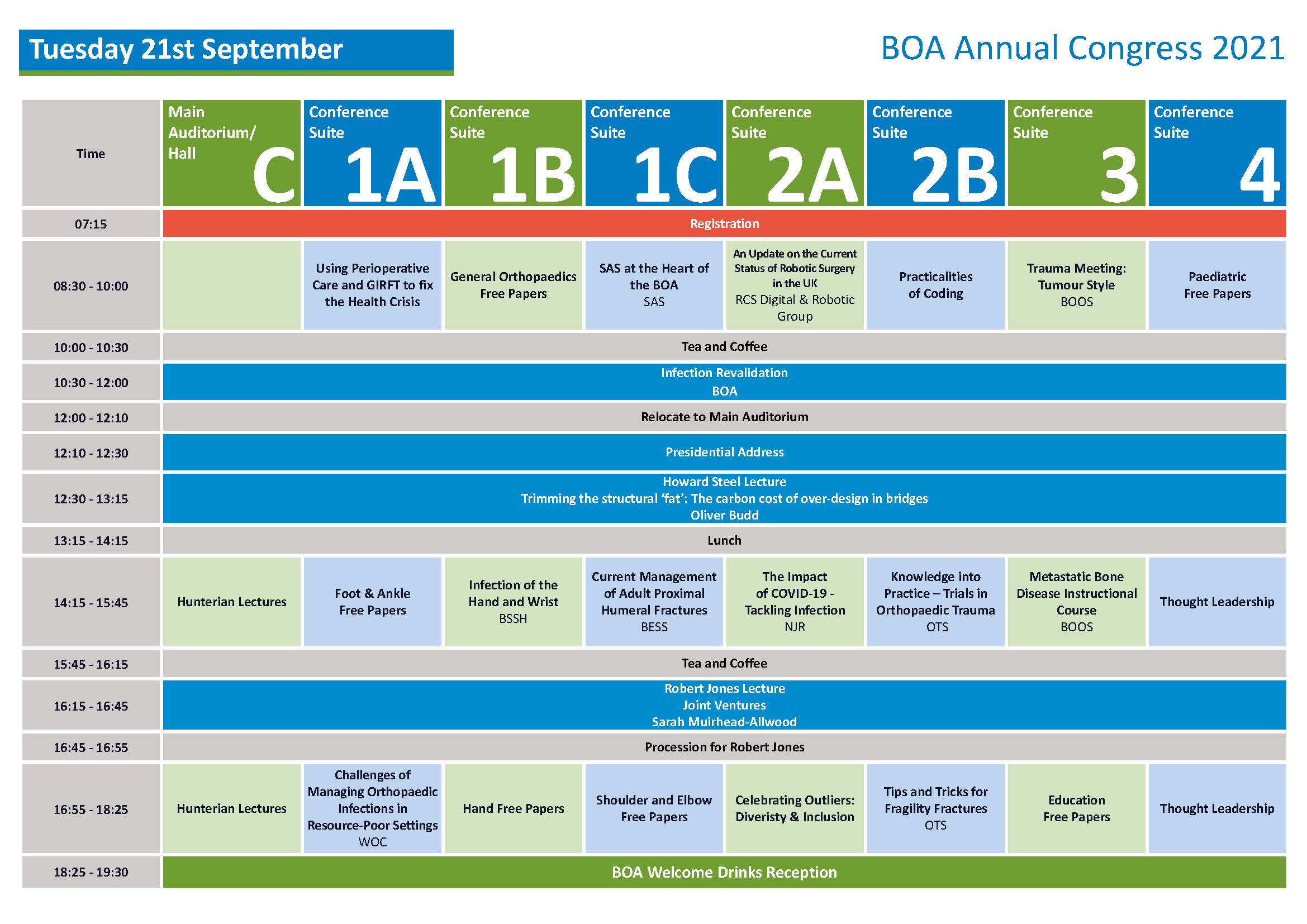
08:30 - 10:00 Using Perioperative Care and GIRFT to Fix the Health Crisis
The desperately long waiting lists following the pandemic give an opportunity to do things better. Perioperative care is everything from the moment an operation is contemplated through to full recovery.
This session starts the BOA congress and is co-badged with the Centre for Perioperative Care (www.cpoc.org.uk). The aim is to harness massive benefits for each patient and for the service. Clear pathways standardising care involve all staff and identify where a patient needs an individual intervention. A perioperative approach can reduce complications by 30%-80% and length of stay by 1-2 days.
Getting It Right First Time (www.gettingitrightfirsttime.co.uk) has highlighted unwarranted variation in practice and results. GIRFT reported on Orthopaedics in 2015 and 2020, showing individual units their own data and identifying how to aim for top decile working. For Orthopaedic surgeons (Consultants, SAS, Registrars, in training and others) the main issues are: creating pathways, maximising preparation of patients and good team working.
Pathways should be co-designed locally with nurses, geriatricians, anaesthetists, GPs, AHPs, patients and administrative staff. A pathway effectively gives every patient the benefit of a specialist approach even where workforce deficiencies persist.
Most pre-assessment services have evolved, with pockets of excellence. Several interventions, principally smoking cessation and regular exercise can reduce complication rates by up to 50%. Nutrition, alcohol moderation, psychological preparedness, medication review and practical preparedness help and empower patients. Pre-operative assessment and optimisation could be improved, including with virtual surgery schools. Staff should be trained in motivational interviewing and local signposting, for example about the practicalities of cycling or swimming for Orthopaedic patients with difficulty weight-bearing.
A ‘Trans-Disciplinary team’ needs team-working and education - so skills are shared and key steps still occur even if specialist staff are not present.
Please search the CPOC website www.cpoc.org.uk for:
• New Day surgery guideline (from GIRFT, CPOC, BADS)
• New diabetes guideline
• Shared Decision Making – listening to patients expectations and discussing Benefits, Risks, Alternatives and what happens if Nothing is done (BRAN)
• Patient information
• Preparation for surgery
• Evidence reviews
• Pre-operative Assessment and Optimisation Guidance
• Work on frailty, anaemia and working across primary and secondary care.
There is a three-fold variation in proportion of people admitted for surgery, rather than being a day case. New Day Surgery guidance could maximise day surgery, avoiding cancellations or competition for beds, and creating geographically-distinct pathways. Many trauma pathways could be converted to day case. Education, empowerment, pathways, team-working - Perioperative care is key.
Conference Suite 1A
Chaired by Scarlett McNally
Speakers: Dr Kim Russon, Dr Jugdeep Dhesi and Professor Tim Briggs
08:30 - 10:00 General Orthopaedics Free Papers
Conference Suite 1B
Chaired by Simon Hodkinson
08:35 - 08:43 Access and Feasibility of Orthopaedic Training in the Independent Sector - A Deanery’s Experience - Albert Ngu
08:43 - 08:51 A Clinical Complexity Scale Combining Local & Systemic Factors, Identifies A Black Swan Patient Group Not Recognised By The UK National Joint Registry - Sunny Deo
08:51 - 08:59 Efficacy of Vitamin-D supplementation in patients with chronic low back pain - Rahman Rasool Akhtar
08:59 - 09:07 Never Events in Orthopaedics: A Nationwide Data Analysis and Guidance on Preventative Measures - Ahmed Hafez
09:07 - 09:15 Tourniquet Use in Orthopaedics and a Novel Tourniquet Pressure Safety Margin - Abigail Johnson
09:15 - 09:23 Computerised Adaptive Testing Dramatically Reduces the Length of Patient-Reported Hip and Knee Outcome Scores. An analysis of the UK National PROMs programme - Jonathan Evans
09:23 - 09:31 Common elective orthopaedic procedures and their clinical effectiveness: An umbrella review of level 1 evidence - Richard Donovan
09:31 - 09:39 Systematic review on the effectiveness of anti-embolism stockings; a need to re-evaluate the evidence - Mahmoud Awadallah
09:39 - 09:47 Consent Plus - A Cost Consequence Analysis - James Brock
09:47 - 09:55 Factors associated with non-union and its management in Atypical Femur Fractures- A 10-year Retrospective study - Nimesh Nebhani
08:30 - 10:00 SAS at the Heart of the BOA (SAS Revalidation)
The BOA is committed to support all the orthopaedic surgeons including the SAS surgeons and Locally Employed Doctors (LED). They are playing an important role in NHS service delivery. In recent years an increasing number of doctors have chosen to become SAS surgeons rather than enter higher specialty training. Due to the evolving demographic of the medical workforce this trend may continue in future years. SAS surgeons and LED are confident and competent healthcare professionals, delivering clinical services in partnership with orthopaedic consultants and other health workers.
They are a diverse group with a wide range of knowledge, surgical skills and experience from novice to expert. Sustaining good quality services to NHS patients requires SAS surgeons to remain up to date with advances in trauma and orthopaedic surgery. Therefore, meeting the professional development needs of SAS surgeons is vital at organisational and individual level. For successful SAS surgeon’s development, appropriate training, and regular assessment linked to the annual appraisal should lead to satisfactory career development.
CESR is not a route for everyone. Do you really want this? If you are happy in your current grade as SAS surgeon and with what you are doing, you may want to ask yourself whether it’s worth applying. This session is targeted at SAS surgeons about how to approach the CESR application and overcome its hurdles to be successful. The CESR route will be presented by the SAC committee members who directly deal with T&O CESR applications.
Conference Suite 1C
Chaired by Mamdouh Morgan
Agenda:
08:30 - 08:35 Welcome & Introduction Mamdouh Morgan08:35 - 08:55 SAS at the Heart of BOA Professor Deborah Eastwood
08:55 - 09:15 New Educational Programme for SAS Surgeon Professor Grey Giddins
09:15 - 09:35 CESR: What, How & When – Is it for me? Deepa Bose
09:35 - 10:00 Questions & Answers
08:30 - 10:00 An update on the current status of robotic surgery in the UK (RCS Digital & Robotic Group)
This session will provide an update on the current value proposition, evidence and research in progress in robotic MSK surgery with a general summary of the activities of the RCS robotic and digital group and updates on current thinking and future directions in hip, knee and spinal surgery.
Conference Suite 2A
Chaired by Professor Fares Haddad
Co-Chaired by Professor Andy Toms
Speakers: Professor David Beard, Mark Blyth, Andrew Metcalfe, Chloe Scott, Peter Wall and Khai Lam
Agenda:
08:30 - 08:35 Introduction Professor Fares Haddad and Professor Andy Toms
08:35 - 08:45 The RCS Robotic and digital strategy Professor David Beard
08:45 - 08:50 Discussion
08:50 - 09:00 Knee – value proposition and options Mark Blyth
09:00 - 09:10 Hip – value proposition and options Chloe Scott
09:10 - 09:20 Discussion
09:20 - 09:30 Knee – Current and future research Andrew Metcalfe
09:30 - 09:40 Hip – Current and future research Peter Wall
09:40 - 09:45 Discussion
09:45 - 09:55 Spine – value proposition and options Khai Lam
09:55 - 10:00 Discussion
08:30 - 10:00 Practicalities of Coding
Whilst the role of the clinician in the current healthcare climate remains as important as ever the data challenges for the future clinician are a daunting prospect. Clinicians have generally shied away from what appears to be a very unfriendly, complex and confusing set of rules, coding systems and payment methodologies used by the NHS to identify activity and appropriately fund it. However, for the success of healthcare delivery it is imperative that there is engagement between clinicians and managers, economists and policy makers.
This session attempts to unravel the mysteries of how the words you “write” are translated into payment decisions for the work you do, policy regarding healthcare service redesign, current and future resource implications, and funding sustainability in an environment where informatics is key and resources are limited. Translating the patient journey from presentation and diagnosis, through to treatment and a (hopefully) positive patient outcome, this session will equip you with an understanding of how clinical records are transformed into data used to make current and future funding decisions regarding the healthcare services you wish to provide for the patient population you serve.
Conference Suite 2B
Chaired by Rohit Kulkarni and Ashley Cole
Agenda:
08:30 - 08:35 Welcome and Introduction Rohit Kulkarni
08:35 - 08:50 A patient’s data journey to getting paid correctly Ashley Cole
08:50 - 09:00 Coding – ICD and OPCS Rohit Kulkarni
09:00 - 09:15 Counting Spells and FCEs, Grouping and HRGs Ashley Cole
09:15 - 09:30 EBI Rohit Kulkarni
09:30 - 09:45 Best practice tariff and specialised commission Ashley Cole
09:45 - 10:00 Blended extended tariff Rohit Kulkarni
08:30 - 10:00 Trauma Meeting: Tumour Style (BOOS Revalidation)
This session will highlight the sort of tumour cases that you may run into in a typical trauma meeting (or FRCS(Tr. & Orth.) Viva.
Cases will be interactive and cover diagnosis and management.
Conference Suite 3
Chaired by Louise McCullough
Speaker: Robert Ashford
08:30 - 10:00 Paediatric Free Papers
Conference Suite 4
Chair: Anish Sanghrajka and Roger Walton
08:35 - 08:43 Can the Physiological Vulnerability Score predict outcomes of hip reconstruction in children with severe neuromuscular disability? - Stephanie Buchan
08:43 - 08:51 The functional mobility of patients with cerebral palsy at long-term follow-up after single-event multilevel surgery - Tomos Edwards
08:51 - 08:59 Prophylactic pinning in Slipped Upper Femoral Epiphysis – a closed loop audit of 25 years practice - Jamie MacLean
08:59 - 09:07 Is Gallows traction effective before open reduction surgery for hip dysplasia? - Stephanie Buchan
09:07 - 09:15 Correlating Patient-Reported Outcome Measures with Radiographic Hip Shape in Perthes' Disease - Mohammed Ali
09:15 - 09:23 Leg length difference in Legg-Calvé-Perthes disease; changes in femoral morphology and the role of contralateral epiphysiodesis - Deborah Eastwood
09:23 - 09:31 Dynamic Supination in Congenital Clubfoot: A Delphi Panel Approach to Standardizing Definitions and Indications for Treatment - Deborah Eastwood
Additional presentation:
09:31 BSCOS consensus guidelines for the management of CTEV in children up to walking age Sally Tenant (on behalf of the BSCOS CTEV consensus group).
10:30 - 12:00 Infection Introduction
The theme of the whole Congress is infection, the objective for this session is to provide an early foundation and some revision. The topics are the common and important, those related to current guidelines or both. To cover such a wide range of subject matter the content of each presentation will be brief and but will signpost further information. The topics will include the following:
- Definition of infection
- Prevention of infection
- Theatre design and use
- Open fractures
- Prophylactic antibiotics
- Spinal infection for the generalist
- The red wound
- The Hot Joint BOAST
- Sampling - how to take intra-operative samples and why
- Necrotising fasciitis
Main Auditorium
Chaired by Professor Bob Handley
Speakers: Matt Scarborough, Andrew Thomas, Ashley Cole, Jamie Ferguson, Deborah Eastwood and Marina Morgan
Agenda:
10:30 - 10:35 Introduction Bob Handley
10:35 - 10:40 Definition of infection Matt Scarborough
10:40 - 10:45 Prevention – Theatre design and use Andrew Thomas
10:45 - 10:50 Open fractures BOAST and NICE Bob Handley
10:50 - 10:55 Prophylactic Antibiotics Matt Scarborough
10:55 - 11:05 Spinal infection for the generalist Ashley Cole
11:05 - 11:10 The red wound – how to deal with a red wound post-op Jamie Ferguson
11:10 - 11:15 Hot joint – BOAST- Standards for care of native hot joint Deborah Eastwood
11:15 - 11:20 Sampling – How to take intra-operative sample and why Jamie Ferguson
11:20 - 11:30 Necrotising fasciitis Marina Morgan
11:30 Closure Bob Handley
12:10 - 12:30 Presidential Address
12:30 - 13:15 Howard Steel Lecture: Trimming the structural ‘fat’: The carbon cost of over-design in bridges
In 2019 the UK Government enshrined in law the requirement to bring all greenhouse emissions to net zero by 2050. For this target to be met, all industrial areas need to reconsider the way they operate. This session will examine future trends in bridge engineering and what bridge designers can do to reduce the embodied carbon (CO₂e) of the structures they design.
Infrastructure accounts for 13% of global cement use. While small compared to buildings (83%), it is also one of the most difficult industrial sectors to fully decarbonise. While use of structural alternatives such as timber is growing in building design, such practice is difficult to replicate in bridges. Bridges are designed for a 120 year design life and require - and will continue to require - durable materials like concrete. A high proportion of process emissions from concrete can only be offset through carbon capture, a technology which remains unproven. This means the civil engineer's role in reducing emissions through design efficiency is vital.
Main Auditorium
Speaker: Oliver Budd
14:15 - 15:45 Hunterian Lectureships
Main Auditorium
Chaired by Anandu Nanu
Agenda:
14:15 - 14:45 The Posterior Malleolar Fracture - An Evolution Lyndon Mason
14:45 - 15:15 Investigations of the mechanisms of infection in Ultra Clean Air Operating Theatres Andrew Thomas
15:15 - 15:45 The WHiTE hip fracture studies: the ghosts of past, present and future Xavier Griffin
14:15 - 15:45 Foot & Ankle Free Papers
Conference Suite 1A
Chaired by Jit Mangwani
14:20 - 14:28 Achilles Tendinopathy Management (ATM): A single blinded placebo controlled multicentre randomised clinical trial of Platelet Rich Plasma Injections for midportion Achilles tendinopathy - Rebecca Kearney
14:28 - 14:36 Is there a reduction in perioperative COVID-19 infection in patients undergoing foot and ankle surgery in designated COVID-19 green pathways? Results from Phase 1 and 2 of the UK Foot and Ankle COVID-19 National (UK-FAlCoN) Audit - Jitendra Mangwani
14:36 - 14:44 Functional outcome of early weight bearing on conservatively managed complete achilles tendon rupture - Rajib Naskar
14:44 - 14:52 Elective removal of metalwork following Lisfranc injury fixation: Results of a national consensus survey of practice - Louise McMenemy
14:52 - 15:00 Outcomes of Posterior Malleolar Fixation in Adult Ankle Fractures in a Major Trauma Centre - Nelson Bua
15:00 - 15:08 Comparison of 3D Surface Rendering CT to Plain Lateral Radiographs for Quantification and Characterisation of Posterior Malleolar Fracture Fragment Size and Morphology - Howard Stringer
15:08 - 15:16 Do baseline patient-reported outcomes predict outcome in Hallux Valgus correction? An analysis of 1015 consecutive cases - Nicholas Hutt
15:16 - 15:24 Management of Open versus Closed Pilon fractures : Comparison of Outcomes and Complications - Victor Lu
15:24 - 15:32 Quantitative assessment of dorsal sagittal lateral column instability in unilateral adult acquired flatfoot deformity (AAFD) - David Chrastek
15:32 - 15:40 The Use of Intramedullary Devices for Fixation of Metatarsal Osteotomies in Hallux Valgus Surgery – A Systematic Review - Amit Zaveri
15:40 - 15:48 First metatarsal rotation and hindfoot alignment in patients with hallux valgus - Ali Asgar Najefi
14:15 - 15:45 Infection of the Hand and Wrist (BSSH)
Chondral and osteochondral lesions represent a difficult treatment problem for the Sport’s Surgeon. There is no uniform approach to managing these patients. In this session we will explore the presentation and the different management options available. We will see how this problem affects various joints commonly affected by sport.
Conference Suite 1B
Chaired by Nicholas Riley
Speakers: Claire Simpson, David Lawrie, Clare Langley and Ian McNab
Agenda:
14:15 - 14:30 Hand anatomy with relevance to infection Claire Simpson
14:30 - 14:40 Questions
14:40 - 14:55 Unusual infections of the hand David Lawrie
14:55 - 15:05 Questions
15:05 - 15:45 Interactive panel discussion of interesting cases Clare Langley, David Lawrie, Ian McNab, Nicholas Riley and Claire Simpson
14:15 - 15:45 Current Management of Adult Proximal Humeral Fractures (BESS Revalidation)
An overview of current management including non-operative management and surgical options of arthroplasty and osteosynthesis.
Conference Suite 1C
Chaired by Amol Tambe
Co-Chaired by Mark Pritchard
Speakers: Rohit Gupta, Benjamin Ollivere, Andrew Brooksbank and Radhakant Pandey
Agenda:
Introduction and Session Outline Amol Tambe (2 minutes)
Cases Amol Tambe and Mark Pritchard (15 minutes)
Invited Speaker 1: Role of Non-operative management in proximal humerus fractures – is the pendulum swinging back to conservative management? Benjamin Ollivere (12 minutes)
Invited Speaker 2: This fracture needs to be fixed! My indications for ORIF in proximal humerus fractures Andrew Brooksbank (12 minutes)
Invited Speaker 3: The Greater tuberosity fracture - not to be underestimated! Radhakant Pandey (12 minutes)
Invited Speaker 4: Is Reverse the way forward for multi fragmented proximal humerus fracture? Rohit Gupta (12 minutes)
Concluding Panel Discussion and Q&A (20 minutes)
14:15 - 15:45 The Impact of COVID-19 - Tackling Infection (NJR)
The National Joint Registry Session will address the vast impact of COVID-19 on volume of orthopaedic surgery procedures during 2020, with specific focus on an analysis of the volume data and what recovery for the sector might involve, as well as its impact on growing waiting lists -with some personal patient perspectives on uncertainty, ongoing pain and experience of surgery during the pandemic.
The second part of the session will focus on the Congress theme: ‘Tackling Infection’, including a presentation on work using NJR data.
Conference Suite 2A
Chaired by Tim Wilton
Speakers: Tim Wilton, Professor Mike Reed, Derek Pegg, Dr Adrian Sayers, Gillian Coward, Deborah Eastwood, Robin Brittain, Ajay Malviya and Professor Michael Whitehouse
Agenda:
14:15 Welcome and Introduction to the NJR Session and Launch of NJR Annual Report Tim Wilton and Professor Mike Reed
What’s new? The benefits the NJR provides to the orthopaedic sector
14:40 COVID-19 - The extent of the impact on the orthopaedic sector Derek Pegg and Dr Adrian Sayers
14:55 Patient perspective of COVID-19 Robin Brittain
15:01 ‘Patient on the waiting list’ - video: patient experiences of the impact of COVID Gillian Coward and Robin Brittain
Introduction to video to highlight the issues around growing waiting lists
15:10 Caring for Patients on the waiting list Professor Deborah Eastwood
15:15 Audience Discussion - COVID-19 impact Derek Pegg, Dr Adrian Sayers, Robin Brittain & Deborah Eastwood with Tim Wilton & Mike Reed
15:25 Role of ceramic bearings in reducing revision for infection after THR Ajay Malviya
15:31 Inpatient and daycase costs for infection after primary hip replacement Professor Michael Whitehouse
Presentation of Paper - an NJR Annual Report 2021 In-depth Research Topic
15:37 Audience Discussion - Tackling Infection Ajay Malviya, Professor Michael Whitehouse with Tim Wilton & Mike Reed
15:43 Chairs’ concluding remarks Tim Wilton
15:45 Session closes
14.15 - 15:45 Knowledge Into Practice – Trials in Orthopaedic Trauma (OTS Revalidation)
Interactive review of current trauma trials. Including presentation of new results and discussion on future projects and collaborations. A comprehensive review contributing towards trauma revalidation.
Conference Suite 2B
Chaired by William Eardley
Speakers: Professor Xavier Griffin, Jamie Ferguson and Professor Joy Adamson
Agenda:
14:15 - 14:20 Introduction William Eardley
14:20 - 14:40 TBC Professor Xavier Griffin
14:40 - 15:00 TBC Professor Joy Adamson (pre-recorded)
15:00 - 15:20 TBC Jamie Ferguson
15:20 - 15:45 Discussion and discussion / promotion of recruiting studies etc. William Eardley
14:15 - 15:45 Metastatic Bone Disease Instructional Course (BOOS Revalidation)
The session will provide an overview on the management of metastatic bone disease, tailored to the learning requirements of the General Orthopaedic Surgeon. The session will focus on investigation, diagnosis, surgical management and patient outcomes and provide a complete overview of the patient with metastatic bone disease.
Conference Suite 3
Chaired by David Boddie
Speaker: Tom Cosker
14:15 - 15:45 Thought Leadership
Conference Suite 4
• 14:15 - 16:00
• 14:15 - 14:35
• 14:40 - 15:00
• 15:05 - 15:25
• 15:30 - 16:00 Innovations in Incision Management: A Case Study Review (Sponsored by 3M)
Chair - Ted O’Connor, 3M Medical Science Liaison
Join Mr Abtin Alvand for the 3M sponsored case review session on “Innovations in Incision Management”
Abtin is a Consultant Orthopaedic Knee Surgeon at the Nuffield Orthopaedic Centre (NOC) and Honorary Senior Clinical Lecturer in Orthopaedic Surgery at the University of Oxford (NDORMS). He graduated from University of London (Guy’s, King’s and St Thomas’ School of Medicine). After completing basic surgical training on the prestigious Hammersmith surgical rotation, he began higher surgical training in Trauma and Orthopaedics on the Oxford programme in 2008. He took three years out of programme to undertake a PhD (DPhil) as the NIHR Biomedical Research Unit Fellow at the University of Oxford. His DPhil was titled “Improving Surgical Learning and Performance at Unicompartmental Knee Arthroplasty”
Abtin was appointed as NIHR Academic Clinical Lecturer at the University of Oxford in 2015, and Honorary Senior Clinical Lecturer in 2017. He undertook two post-CCT sub-specialist clinical fellowships focusing on complex hip and knee surgery in Oxford (NOC) and Stanmore (Royal National Orthopaedic Hospital). He was then appointed in Oxford as a Consultant Orthopaedic Knee Surgeon. Clinically, he has a specialist interest in unicompartmental knee arthroplasty, revision knee arthroplasty, and peri-prosthetic joint infection.
16:15 - 16:45 Joint Ventures (Robert Jones Lecture)
This talk will focus on the value and importance of orthopaedic surgeons collaborating with engineers and other scientific disciplines to further improve orthopaedics.
Main Auditorium
Chaired by John Skinner
Speaker: Sarah Muirhead-Allwood
16:55 - 18:25 Hunterian Lectureships
Main Auditorium
Chaired by Anandu Nanu
Agenda:
16:55 - 17:25 Improving hip fracture outcomes using routinely collected health data David Metcalfe
17:25 - 17:55 Unicompartmental Knee Replacement Professor David Murray
17:55 - 18:25 Evaluating the Role of Novel Technologies in Optimising Arthroscopic Management of Femoroacetabular Impingement Vikas Khanduja
16:55 - 18:25 Challenges of managing orthopaedic infections in resource-poor settings (WOC Revalidation)
This session will include insights into the management of orthopaedic infections in low and middle income countries. Free papers on Developing World Orthopaedics will also be presented.
Conference Suite 1A
Chaired by Deepa Bose
Co-Chaired by Alberto Gregori
Agenda:
16:55 - 17:40 Free papers (Developing World Orthopaedics)
17:40 - 17:55 Orthopaedic surgery in HIV positive patients in resource-poor settings Simon Graham
17:55 - 18:10 The Beit-Cure classification of childhood osteomyelitis Jim Harrison
18:10 - 18:25 Challenges in the management of chronic osteomyelitis in Ethiopia Alwyn Abraham
18:25 - 18:40 Management of spinal tuberculosis in Malawi Professor Shanmuganathan Rajasekaran & Ashtin Doorgakant
Free Papers:
17:00 - 17:08 Mechanical Testing of the Jaipur Foot against low, mid and high activity prosthetic feet - Jeremy Telford
17:08 - 17:16 Epidemiology of fractures and their treatment in Malawi: Results of a multicentre prospective registry study to guide orthopaedic care planning - Alexander Schade
17:16 - 17:24 Comparative analysis of radiological evaluation and early functional outcome of total knee arthroplasty using accelerometer-based handheld navigation system - Nuthan Jagadeesh
17:24 - 17:32 Does Bone Ninja application can serve as an alternative to PACS to measure preoperative deformity and postoperative alignment measurements in case of total - Nuthan Jagadeesh
17:32 - 17:40 Delayed and late prosthetic joint infections following total knee replacement: a multicenter study of fifteen thousand patients - Darshan Angadi
16:55 - 18:25 BSSH Free Papers
Conference Suite 1B
Chaired by Philippa Rust
Co-chaired by Ian McNab
Agenda:
17:00 - 17:08 Articular cartilage and soft tissue damage from radiofrequency thermal ablation wands at wrist arthroscopy Grey Giddins
17:08 - 17:16 The management of suspected scaphoid fractures in the United Kingdom: a national cross-sectional study Ben Dean
17:16 - 17:24 Association of trapeziometacarpal joint shape with clinical symptoms and radiological severity of thumb base osteoarthritis: Analysis of a cohort from the osteoarthritis initiative study using a statistical shape model Anna Riemen
17:24 - 17:32 The Value of Calibration of Radiographs in Total Wrist Arthroplasty Nastaran Sargazi
17:32 - 17:40 The Aberdeen outpatient dedicated percutaneous needle fasciotomy clinic for the treatment of Dupuytren’s Disease. A valuable resource in the re-establishment of orthopaedic service following the coronavirus pandemic Yasmeen Khan
17:40 - 17:45 Free
17:45 - 17:53 A Meta-Analysis of Proximal Scaphoid Fractures - Does Terminology Affects Reported Union Rates? Han Hong Chong
17:53 - 18:01 Cone-beam CT in the diagnosis of radiocarpal fractures: A Systematic Review and Meta-analysis Emma Fitzpatrick
18:01 - 18:09 Delaying fixation of distal radius fractures beyond the best practice guidelines does not affect the final outcome Sanjay Chilbule
18:09 - 18:17 A case series of patients treated with percutaneous intramedullary screws, for 5th metacarpal fractures, using the WALANT technique at Hinchingbrooke Hospital Nauful Ahmed
18:17 - 18:25 Custom-Fashioned Antibiotic Impregnated PMMA MCP Joint Arthroplasty in the Acute Settling Long Term Outcome: A Novel Technique Revisited: Our Own Experience Frances Bowerman
16:55 - 18:25 Shoulder and Elbow Free Papers (BESS)
Conference Suite 1C
Chaired by Mark Pritchard
Co-Chaired by Addie Majed
17:00 - 17:07 Anterior Instability of the Sternoclavicular Joint: Long Term Results from a Tertiary Center in the United Kingdom - Lambros Athanatos
17:07 - 17:14 Clinical Results and 10-Year Survivorship of the Synthes Epoca Resurfacing Head Total Shoulder Arthroplasty - Timothy Karssiens
17:14 - 17:21 Diabetes and outcomes following reverse polarity shoulder arthroplasty- a single centre experience - Hasan Daoud
17:21 - 17:28 Elbow Hemiarthroplasty has Equivalent Functional Outcomes and a Lower Early Complication Rate Compared to Open Reduction Internal Fixation for Treatment of Multi-fragmentary Distal Humeral Fracture in Patients >60 Years of Age - Anand Tathgar
17:28 - 17:35 Radial Head Arthroplasty for Trauma: Medium to long term outcomes of press-fit radial head arthroplasty - Pradeep Kankanalu
17:35 - 17:42 Patient-specific instrumentation versus standard surgical instruments in primary reverse total shoulder arthroplasty: A retrospective clinical comparative study - Ahmed Elsheikh
17:42 - 17:49 Does the addition of cross-element fixation prevent locking screw subsidence following plate fixation of proximal humerus fractures? Priyadarshi Amit
17:49 - 17:56 Validation of the Radiographic Union Score for HUmeral fractures (RUSHU): a retrospective study in an independent centre - William Fordyce
17:56 - 18:03 Long-Term Outcomes Following Manipulation Under Anaesthetic for Patients with Frozen Shoulder - Dr Thomas Davies
16:55 - 18:25 Celebrating Outliers: Diversity & Inclusion
The organisers of the diversity session have asked if you would complete a quick poll around diversity to give them '3 words that best describe you'. Please click the link below or access the QR code to participate.
A session celebrating diversity in orthopaedics. This session will present and agree action points for widening participation in diversity initiatives supporting current and future trainees and consultants. Baroness Helena Kennedy QC will present the key findings of her diversity and inclusion (D&I) report for RCS England. Additionally, we will review data from the BOA’s recent diversity and inclusion survey, explore ways to promote new recruits, hear of the effects of ethnicity on patient experience and outcomes, and agree areas for future BOA research.
Conference Suite 2A
Chaired by Caroline Hing
Co-Chaired by Chloe Scott and Matthew Brown
Speakers: Helena Kennedy, Caroline Hing, Salma Chaudhury, Fergal Monsell, Suddhajit Sen and Sarah Stapley
Agenda:
16:55 - 17:05 Introduction Chloe Scott & Matthew Brown
- Welcome and outline of session
- Three words that best describe you
17:05 - 17:20 BOA Diversity and Inclusion Survey and Strategy Caroline Hing & Salma Chaudhury
- Presentation of BOA D&I Survey data
- Key findings
- Action points
- Summary and update on current and future BOA D&I plans
- Introduction to priority setting
17:20 - 17:40 The Kennedy Report Baroness Helena Kennedy QC
- Presentation of RCS England Kennedy Report
- Key findings and action points
17:40 - 17:55 Undergraduate Diversity Fergal Monsell
- Inspiring the next generation of orthopaedic surgeons
17:55 - 18:05 Promoting cultural diversity for better patient care Suddhajit Sen
- Discussing the effect of ethnicity on patient care
18:05 - 18:15 A diverse and happy training programme Sarah Stapley
- Wessex TPD shares her experience of a diverse training programme
18:15 - 18:20 Priority Setting Vote Chloe Scott
- Vote on top 5 areas for focus of future research
18:20 - 18:30 Discussion and Sign-Posting Chloe Scott
- Sign-posting to resources
- Social media
16:55 - 18:25 Tips and tricks for fragility fractures (OTS Revalidation)
Case based session generating debate on how to manage the increasing number of fragility fractures. New concepts, techniques and kit will be discussed, with a focus on fractures around the knee. Tips and tricks for more challenging fractures will be presented as an update for trauma revalidation.
Conference Suite 2B
Chaired by Jayne Ward
Co-Chaired by Mike Kelly
Speakers: Sunit Patel, Mateen Arastu and Jim McVie
16:55 - 18:25 Education Free Papers
Conference Suite 3
Chaired by Simon Hodkinson
17:00 - 17:08 Teaching large joint clinical examination: Is there a role for educational videos to augment teaching? A randomised single blinded control trial - Elinor Flatt
17:08 - 17:16 The influence of Gender on Operative Autonomy in Surgical Training (GOAST) – Regional Pilot Study - Jennifer Cherry
17:16 - 17:24 Pathways to Competence: Exploring the Basis of Operative Competency Decisions in Trauma & Orthopaedic Training - Simon Fleming
17:24 - 17:32 Whichdeanery.com – a useful resource for those applying to T&O specialty training - Amit Chawla
17:32 - 17:40 Planning and delivering a BOA Specialty Society Diversity and Inclusion survey - Simon Britten
17:40 - 17:48 RLHOTS Mentorship Programme For Medical Students Improved Students Interest in Orthopaedics - David Ensor
17:48 - 17:56 UK Orthopaedic trainees covering medical Covid-19 wards and still meet Joint Committee on Surgical Training trauma procedure guidelines: A successful multifaceted collaborative model - David Ferguson
17:56 - 18:04 Virtual Orthopaedic Trainee Education: Lessons learnt during COVID-19 - Rosie Hackney
16:55 - 18:25 Thought Leadership
Conference Suite 4
Agenda:
16:55 - 17:15 AgNovos: Current Epidemiological Trends in Fragility Hip Fractures in the UK
Chaired by Falk Dukatz
Overview of Effectiveness and Gaps in Current Mitigation Strategies to Address Secondary Risk in the UK - Dr Andrew David Duckworth (pre-recorded)
• Pharmacologic Treatment
• Coordination of Care (i.e., FLS)
Novel Emerging Approaches to Address Secondary Risk of Hip Fractures - Professor Benjamin Ollivere (pre-recorded)
• Surgical Treatment
• RESTORE Study
17:20 - 17:40 Innovations in Incision Management: A Case Study Review (Sponsored by 3M)
Chair - Ted O’Connor, 3M Medical Science Liaison
Join Mr Abtin Alvand for the 3M sponsored case review session on “Innovations in Incision Management”
Abtin is a Consultant Orthopaedic Knee Surgeon at the Nuffield Orthopaedic Centre (NOC) and Honorary Senior Clinical Lecturer in Orthopaedic Surgery at the University of Oxford (NDORMS). He graduated from University of London (Guy’s, King’s and St Thomas’ School of Medicine). After completing basic surgical training on the prestigious Hammersmith surgical rotation, he began higher surgical training in Trauma and Orthopaedics on the Oxford programme in 2008. He took three years out of programme to undertake a PhD (DPhil) as the NIHR Biomedical Research Unit Fellow at the University of Oxford. His DPhil was titled “Improving Surgical Learning and Performance at Unicompartmental Knee Arthroplasty”
Abtin was appointed as NIHR Academic Clinical Lecturer at the University of Oxford in 2015, and Honorary Senior Clinical Lecturer in 2017. He undertook two post-CCT sub-specialist clinical fellowships focusing on complex hip and knee surgery in Oxford (NOC) and Stanmore (Royal National Orthopaedic Hospital). He was then appointed in Oxford as a Consultant Orthopaedic Knee Surgeon. Clinically, he has a specialist interest in unicompartmental knee arthroplasty, revision knee arthroplasty, and peri-prosthetic joint infection.
17:40 - 18:00
18:00 - 18:30 ARTHROSAMID by Contura Orthopaedics Ltd - The Knee OA Treatment 20 Years in the Making
The Knee OA treatment 20 years in the makingAgenda:
• What are the limitations to treat the fastest growing cause of disabilities worldwide?
• The history of iPAAG – Novel therapy to treat patients with knee OA
• Years of experience in using iPAAG: the benefits I have seen in patients with knee OA
Invited faculty:
• Mr Sean Curry – Consultant Orthopaedic & Trauma Surgeon, UK
• Ieva Ankorina-Stark – Chief Scientific Officer, Contura
• Professor Henning Bliddal – Rheumatologist, Denmark
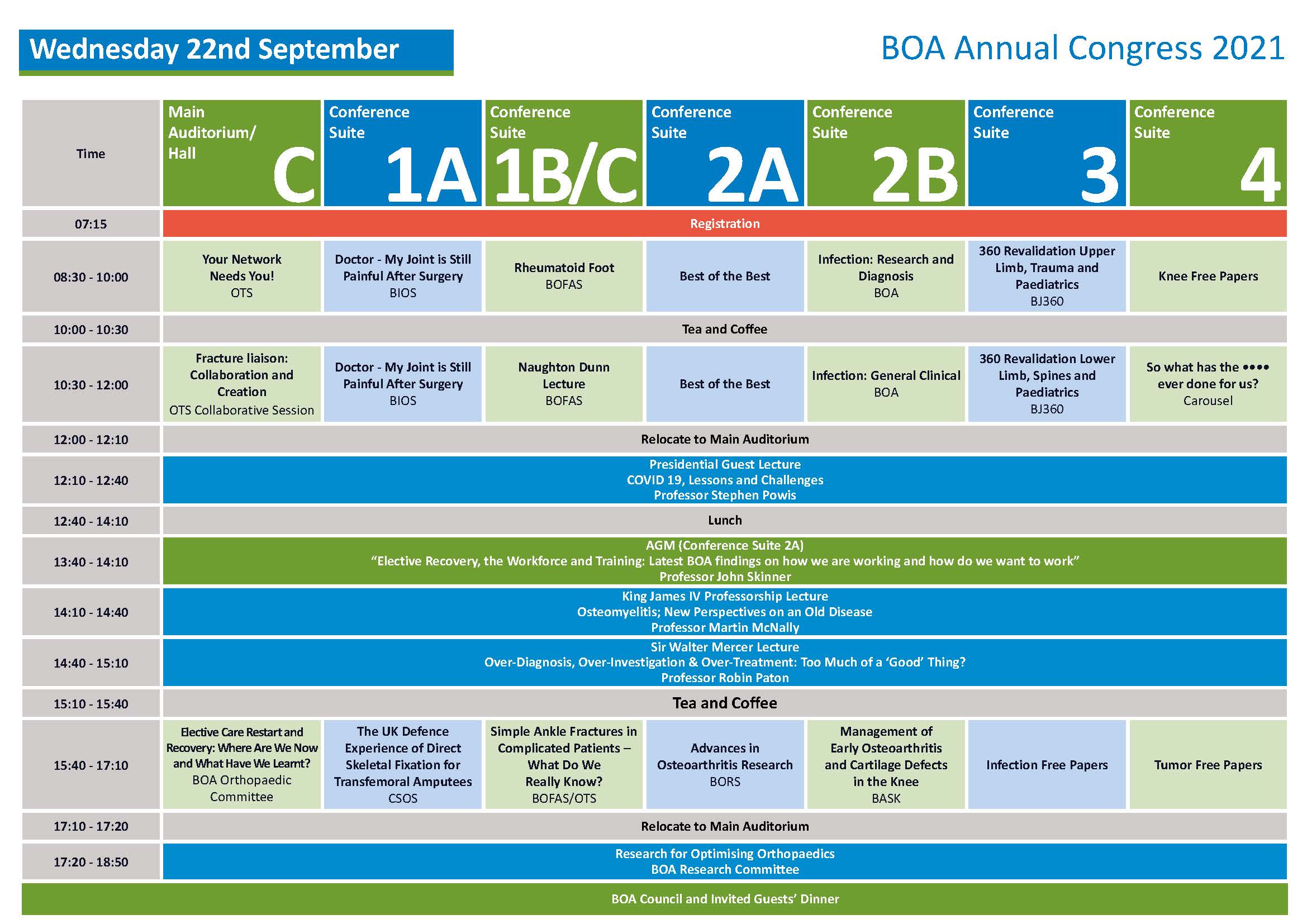
08:30 - 10:00 Your Network Needs You! (OTS Revalidation)
Discussion session with updates on policy and practice from the trauma community. Incorporating the introduction the BOA trauma exchange group. Get involved and influence how trauma is managed in your local trauma network.
Main Auditorium/Hall C
Chaired by Alex Trompeter
Speakers: Bob Handley, Julia Trussler, Sharon Scott, Tom Quick and Jayne Ward
Agenda:
08:30 Introduction Alex Trompeter
08:32 BOAST overview Alex Trompeter and William Eardley
08:35 BOAST update – Arterial injuries Jayne Ward
08:47 BOAST update – Peripheral nerve injury Tom Quick
09.59 BOAST update – Paediatric forearm fracture Fergal Monsell
09:11 Q&A on Part 1 Alex Trompeter
09:20 Part 2 overview Alex Trompeter
09:22 Getting involved – BOA trauma committee Julia Trusler
09:24 Getting involved – Trauma exchange Alex Trompeter
09:26 Developing a career in trauma leadership at a national level Sharon Scott and Bob Handley
09:46 Q&A on Part 2 Alex Trompeter
09:59 Close Alex Trompeter
08:30 - 10:00 Doctor - My joint is still painful after surgery (BIOS Revalidation)
The session aims to explore the causes of postoperative painful joints with an emphasis on infection with a multidisciplinary approach to assessing, investigating and managing such situations. At the end of each section a case based discussion will bring panellists together for expert opinion.
Chaired by Professor Amit Tolat and Professor Bijayendra Singh
Speakers: Professor Simon Lambert, Jitendra Mangwani, Dr Kiran Sachane and Dr Amanda Isaac
Agenda:
08:30 - 08:45 Shoulder Pain after Surgery Professor Simon Lambert08:50 - 09:05 Foot and Ankle Pain after Surgery Jitendra Mangwani
09:10 - 09:25 Pain management – Shoulder/F & A/hand CRPS Dr Kiran Sachane
09:30 - 09:45 Radiology of painful Joints with emphasis on Infection/MDT approach Dr Amanda Isaac
09:50 - 10:00 Case based discussion All
08:30 - 10:00 Rheumatoid Foot (BOFAS Revalidation)
Conference Suite 1B/C
Chaired by Nikki Kelsall
Co-Chaired by Robert Clayton
Agenda:
08:30 Welcome & Introduction Nikki Kelsall
08:35 Clinical assessment & disease pattern in the rheumatoid foot Vivek Dhukaram
08:45 What is rheumatoid arthritis? Do DMARD’s increase infection risk in F&A surgery? Dr Alan Macdonald
08:55 Anaesthetic assessment of the Rheumatoid Patient Dr Colin Patterson
09:05 What are the principles of orthoses in the rheumatoid foot? What should I write on my request form? Effect of foot wear on body image and self esteem Nick Gallogly
09:15 Discussion Nikki Kelsall & Rob Clayton
09:20 Principles of rheumatoid foot surgery Hari Prem
09:30 Hints & Tips – Forefoot surgery and its complications Howard Davies
09:40 Hints & Tips – Ankle replacement surgery and it’s complications Heath Taylor
09:50 Discussion Nikki Kelsall & Rob Clayton
08:30 - 10:00 Best of the Best
Conference Suite 2A
Chaired by Donald M Campbell
08:30 - 08:37 The effect of gender on operative autonomy in surgical training (GOAST) – regional pilot study - Samantha Downie
08:37 - 08:44 Supracondylar fractures of the humerus in children: A five-year retrospective cohort study in a non-paediatric Major Trauma Centre providing dedicated children’s orthopaedic services - Dan Hill
08:44 - 08:51 Intravenous tranexamic acid given at femoral fragility fracture surgery reduces blood transfusion requirements four-fold - Matilda Powell-Bownes
08:51 - 08:58 Percutaneous strain reduction screws are a cost effective and reproducible method to treat long bone non-union - Matthew Bence
08:58 - 09:05 The prevalence and impact of gender bias and sexual discrimination - Ghazal Hodhody
09:05 - 09:12 Does the modified Glasgow Prognostic Score aid in the management of patients undergoing surgery for a soft tissue sarcoma? An international multi-centre study - Omer Alanie
09:12 - 09:19 Coronavirus infection in Hip Fractures (CHIP) Study A case matched multi-centre study of 1633 hip fracture patients - Fatima Rashid
09:19 - 09:26 The Edmonton Frail Scale (EFS) as a predictor of post-operative outcomes in elective total hip and knee replacement surgery - Gopikanthan Manoharan
09:26 - 09:33 A Video Analysis of Distal Bicep Tendon Ruptures: Challenging The Traditionally Accepted Mechanism of Injury - Chris Jukes
09:33 - 09:40 Peri-operative administration of tranexamic acid in lower limb arthroplasty: a multicentre, prospective cohort study - Thomas Lloyd
09:40 - 09:47 Mortality Following Fractured Neck of Femur in The Peri-centenarian Population - Moritz Lebe
09:47 - 09:54 Evaluating the role of Carbon Fibre Reinforced Polyetheretherketone and titanium intramedullary nails in patients with metastatic bone disease - Aashish Ahluwalia
09:54 - 10:01 A five-year review comparing 30-day mortality following intramedullary nailing versus sliding hip screw for trochanteric hip fractures - Gavin Baker
08:30 - 10:00 Infection - Research and Diagnosis
Conference Suite 2B
Chaired by Professor Mike Reed
Co-Chaired by Rhidian Morgan Jones and Professor Andrew Toms
Speakers: Professor Grant Burgess, Professor Andrew Toms, Matt Scarborough and Iain McNamara
Agenda:
08:30 - 08:31 Open Professor Mike Reed
08:31 - 08:51 Multidisciplinary working Dr Matt Scarborough
08:51 - 09:11 Biofilms & Marine Endonucleases: what you should know! Professor Grant Burgess
09:11 - 09:21 BOAST Rev TKR diagnosis Professor Andrew Toms
09:21 - 09:31 Calprotectin Professor Iain McNamara
09:31 - 09:51 Diagnostics update Dr Javad Parvizi
09:51 - 10:00 Questions and Answers
10:00 End
08:30 - 10:00 360 Revalidation Upper Limb, Trauma and Paediatrics (BJ360)
A whistle stop tour of everything new, important and controversial in orthopaedics that involves the upper limb (and paediatrics) and trauma. From the latest RCT to can't miss policy papers. This lighthearted and informative session has become a staple of the BOA. We look forward to seeing you there.
Conference Suite 3
Chaired by Professor Xavier Griffin
Speakers: Andrew Duckworth, Helen Chase and Professor Xavier Griffin
Agenda:
8:30 - 8:45 Introduction and upper limb trauma Professor Benjamin Ollivere
8:50 - 9:10 Upper limb essential papers Andrew Duckworth
9:15 - 9:30 Paediatrics 101 Helen Chase
9:35 - 9:50 Trials and tribulations in Trauma Professor Xavier Griffin
08:30 - 10:00 Knee Free Papers
Conference Suite 4
Chaired by Leela Biant
08:43 - 08:51 The effect of the use and type of patella component on ODEP ratings of total knee prostheses - Pradyumna Raval
08:51 - 08:59 Oxford Unicompartmental Knee Arthroplasty Versus Total Knee Arthroplasty - Long term functional outcomes and survival analysis - Elizabeth Lindsay
08:59 - 09:07 Inflammatory Response in Robotic Total Knee Arthroplasty versus conventional Jig-based and the correlation with Early Functional Outcomes: Results of a Prospective Randomised Controlled Trial - Andreas Fontalis
09:07 - 09:15 Applicability of the specific criteria for problematic knee replacement following revision TKA. Influence of diagnosis on mid-term outcomes - Andrew Jones
09:15 - 09:23 Does the RKCC classification predict the true cost of revision knee arthroplasty? A financial analysis of eighty-nine cases at a regional centre - Aris Alexiadis
09:23 - 09:31 No difference of gait parameters in patients with image-free robotic-assisted medial unicompartmental knee arthroplasty compared to a conventional technique: a randomized controlled trial - Cécile Batailler
09:31 - 09:39 A matched comparison of the long term outcomes of cemented and cementless total knee replacements, based on data from the national databases: An analysis from the National Joint Registry of England, Wales, Northern Ireland and Isle of Man - Hasan Mohammad
09:39 - 09:47 Provision of Revision Knee Arthroplasty services across Scotland: A national audit - Luke Farrow
09:47 - 09:55 Differences in Early Recovery following Unicompartmental Knee Replacement with Daycase and Standard Care Pathways, assessed using the Oxford Arthroplasty Early Recovery Score (OARS) - Azmi Rahman
10:30 - 12:00 Fracture liaison: Collaboration and Creation (OTS Collaborative)
Collaborative session introducing the fracture liaison academy and network.
Topics include:
- Secondary fracture prevention for the trauma team - opportunities for getting started and becoming more effective
- Global Progress in Fragility Fracture
- Life is kyphogenic; the effects of age and fragility on the spine
- Operative techniques in fragility fractures
- Toolkits to enhance fracture liaison success
Main Auditorim/Hall C
Chaired by Andrew Gray
Speakers: Dr Kassim Javaid, Professor David Marsh, Lee Breakwell, William Eardley and Paul Mitchell
10:30 - 12:00 Doctor - My joint is still painful after surgery (BIOS Revalidation)
The session aims to explore the causes of postoperative painful joints with an emphasis on infection with a multidisciplinary approach to assessing, investigating and managing such situations. At the end of each section a case based discussion will bring panellists together for expert opinion.
Conference Suite 1A
Chaired by Sanjeev Anand and Sunil Garg
Speakers: Nikhil Shah, Peter James, Dr Raja Reddy and Dr Bridget Atkins
Agenda:
10:30 - 10:45 Hip Pain after Surgery/ Revision Surgery Nikhil Shah + 5 minute discussion
10:50 - 11:05 Knee Pain after Surgery/Revision Surgery Peter James + 5 minute discussion
11:10 - 11:25 Pain management after Hip/knee Surgery Dr Raja Reddy + 5 minute discussion
11:30 - 11:45 Microbiologist approach to Infected joints postoperative setting / MDT approach Dr Bridget Atkins + 5 minute discussion
11:50 - 12:00 Case based discussion All
10:30 - 12:00 The Naughton Dunn Lecture - Foot & Ankle Surgery in the UK - Past, Present & Future (BOFAS)
Conference Suite 1B/C
Chaired by Nikki Kelsall
Co-Chaired by Heath Taylor
Speaker: Simon Hodkinson
10:30 - 12:00 Best of the Best
Conference Suite 2A
Chaired by Donald M Campbell
10:30 - 10:37 Provision of Revision Knee Arthroplasty services across Scotland: A national audit - Luke Farrow
10:37 - 10:44 Safety of emergency, elective and day case operating during the winter period at East Suffolk and North Essex NHS Foundation Trust: lessons from the outcomes of 4,254 surgical patients from the first COVID-19 wave - Sunny Parikh
10:44 - 10:51 JSES Reviews, Reports, and Techniques - Eilis Fitzgerald
10:51 - 10:58 Dual Mobility Cup Versus Conventional Total Hip Arthroplasty for Femoral Neck Fractures: An International Multi-Registry Study - James Masters
10:58 - 11:05 Elective Total Hip Arthroplasty in patients with neurodegenerative disorders and epilepsy: A report of 2,860 cases from the Swedish Hip Arthroplasty Register - Atanu Bhattacharjee
11:05 - 11:12 Sulphur Biology in Skeletal Development: An Explorative Study into the Aetiology of Developmental Dysplasia of the Hip - Amanda Rhodes
11:12 - 11:19 Cost utility analysis of bilateral osseointegration for trans-femoral amputations in military blast injury - Charles Handford
11:19 - 11:26 Helicopter and ground emergency medical services transportation to hospital after major trauma in England, a comparative cohort study - Oliver Beaumont
11:26 - 11:33 Implementing grip strength assessment to enhance risk stratification in hip fracture patients - Antony Sorial (Shivam Kolhe will be presenting)
11:33 - 11:40 Teaching large joint clinical examination: Is there a role for educational videos to augment teaching? A randomised single blinded control trial - Eli Flatt
11:40 - 11:47 Femoral Head Histology – When is this test useful? - Mohammad Al-Ashqar
11:47 - 11:54 The onset, progress and factors influencing degenerative arthritis of the wrist following scaphoid fracture non-union - Amin Kheiran
10:30 - 12:00 Infection - General Clinical
Conference Suite 2A
Chaired by Professor Andrew Toms
Co-Chaired by Matt Scarborough and Jamie Ferguson
Speakers: Rhidian Morgan Jones, Mario Morgenstern, Benjamin Bloch, Dr Marina Morgan, Andrej Trampuz, Professor Andrew Toms and Professor Mike Reed
Agenda:
10:30 - 10:31 Open Professor Andrew Toms
10:31 - 10:41 How to do a debridement Rhidian Morgan Jones
10:41 - 11:01 An overview of fracture related infection Mario Morgenstern
11:01 - 11:11 Single and two stage revision Benjamin Bloch
11:11 - 11:21 10 things surgeons should know about Microbiology Dr Marina Morgan
11:21 - 11:31 Phage therapy Andrej Trampuz
11:31 - 11:36 Questions and Answers
Referral networks
11:36 - 11:44 Referral networks – update from Revision Knee Working Group Professor Andrew Toms
11:44 - 11:52 Bone and Joint Infection registry and running and auditing the MDT Professor Mike Reed
11:52 - 12:00 Questions and Answers
12:00 End
10:30 - 12:00 360 Revalidation Lower Limb, Spines and Paediatrics (BJ360)
A whistle stop tour of everything new, important and controversial in orthopaedics that involves the upper limb (and paediatrics) and trauma. From the latest RCT to can't miss policy papers. This lighthearted and informative session has become a staple of the BOA. We look forward to seeing you there.
Conference Suite 3
Chaired by Brett Rocos
Speakers: Sebastian Dawson Bowling, Dan Perry, Michael Whitehouse and Brett Rocos
Agenda:
10:30 - 10:45 Introduction and lower limb trauma Professor Benjamin Ollivere
10:45 - 11:00 Papers not to miss in the spine Brett Rocos
11:00 - 11:15 Paeds for beginners Professor Dan Perry
11:15 - 12:00 Hip and Knee Professor Michael Whitehouse & Sebastian Dawson Bowling
10:30 - 12:00 What has the **** ever done for us? (Carousel)
What the Carousel Associations do best, and how they do it.
Conference Suite 4
Chaired by Bob Handley
Speaker: Kishmore Puri, Peter Devane, Michael Gillespie, Brian Bernstein, Serena Hu & Joseph Bosco
12:10 - 12:40 COVID-19; Lessons and Challenges (Presidential Guest Lecture)
Main Auditorium
Speaker: Professor Stephen Powis
13:40 - 14:10 AGM
Conference Suite 2A
Including Presentation from Vice President, Professor John Skinner “Elective Recovery, the Workforce and Training: Latest BOA findings on how we are working and how do we want to work.”
14:10 - 14:40 Osteomyelitis; New Perspectives on an Old Disease (King James IV Professorship)
Main Auditorium
Chaired by Michael Griffin OBE
Speaker: Professor Martin McNally
14:40 - 15:10 Over-diagnosis, over-investigation & over-treatment: Too much of a 'good' thing? (Sir Walter Mercer Lecture)
Main Auditorium
Chaired by Phil Turner
Speaker: Professor Robin Paton
15:30 - 16:30 Tumour Free Papers
Conference Suite 4
Chaired by Tom Cosker and Robert Ashford
15:30 - 15:38 Investigating Mirels’ scoring for Upper Limb Metastasis- Should the cut-off for prophylactic surgery be different? - Katie Hoban
15:38 - 15:46 Retrospective analysis of risk factors for progression to fracture in patients with metastatic bone disease (MBD) - Samantha Downie
15:46 - 15:54 The management of spinal oligometastases at a supra-regional centre in the era of Stereotactic Ablative Radiotherapy - Ben Barkham
15:54 - 16:02 Prediction models for survival, local recurrence and metastases of Leiomyosarcomas of trunk wall and extremities: A multicentre study - Sudhir Kannan
16:02 - 16:10 The Role of Intraoperative Cell Salvage for Musculoskeletal Sarcoma Surgery - Raja Bhaskar
16:10 - 16:18 Incidence of unexpected positive margin following excision of primary bone & soft tissue tumours in a tertiary centre and the impact on patient outcomes - George Matheron
16:18 - 16:26 Tumours of the Proximal Humerus : A Tertiary Referral Centre Experience - Varun Sethurajah
15:40 - 17:10 Elective Care Restart and Recovery: Where are we now and what have we learnt? (BOA Orthopaedic Committee)
While we are all in this together, experiences vary from one region to another. In this session we will explore the current problems in terms of workload and workforce. We will review the situation from our patients’ perspective and will hear of the challenges for our trainees. There have been a variety of national initiatives, local pilots and regional case studies, as well as changes implemented in the heat of the pandemic now being tested in more ‘normal’ service conditions (and more besides!). Learn about what’s been happening around the country in this session and take this chance to consider what might work for you and your team.
Main Auditorium
Chaired by Bob Handley and John Skinner
Speakers: Deborah Eastwood, Andrew Bennett, Tracey Loftis, Arthur Stephen, Oliver Adebayo, Mike Reed, Phil Turner, Mark Bowditch, Tim Briggs and Julian Owen
Agenda:
15:40 - 15:50 Where are we now? Deborah Eastwood
15:50 - 16:00 #BestMSKHealth: How does it help orthopaedic surgeons? Andrew Bennett
16:00 - 16:10 Elective Recovery, the Workforce and Training: Latest BOA findings on how we are working and how we want to work John Skinner
16:10 - 16:15 The Versus Arthritis Patient Survey: How are they and how can we help? Versus Arthritis - Tracey Loftis
16:15 - 16:30 "Surgical Case prioritisation and harm reviews. How, why or even possible?” Arthur Stephen
16:30 - 16:35 BOTA Viewpoint: Service vs Training Oliver Adebayo
16:35 - 16:55 Ideas from around the UK on how to solve the problem of access to care: Local solutions? Mike Reed, Phil Turner, Mark Bowditch, Tim Briggs and Julian Owen
16:55 - 17:10 Q&A
15:40 - 17:10 The UK Defence experience of Direct Skeletal Fixation for transfemoral amputees (CSOS Revalidation)
During the conflicts in Iraq and Afghanistan UK service personnel sustained significant injuries including single, double and triple amputations. These patients have developed significant rehabilitation issues that were unable to be addressed using conventional sockets. UK Defence was awarded LIBOR funding to undertake Direct Skeletal Fixation in twenty patients with femoral amputations who had failed the conventional treatment that was available within the NHS.
Conference Suite 1A
Chaired by Paul Hindle
Co-chaired by Alan Mistlin
Speakers: Alan Mistlin, Paul Hindle, Louise McMenemy, Charles Handford and Andy Reid MBE
The rehabilitation problem Col Alan Mistlin
Direct Skeletal Fixation Wg Cdr Paul Hindle
UK outcome data Surg Lt Cdr Louise McMenemy
Economic case Major Charles Handford
The patient experience Andy Reid MBE
15:40 - 17:10 Simple ankle fractures in complicated patients – what do we really know? (BOFAS/OTS Revalidation)
Conference Suite 1B/C
Chaired by Nikki Kelsall
Co-Chaired by Jayne Ward
Agenda:
15:40 Welcome & Introduction Nikki Kelsall
15:45 All ankle fractures should be assessed with CT scans Anthony Sakellariou
15:55 Elderly patients should all be treated in a plaster (AIM) Matt Solan
16:05 Elderly patients should all be treated with hind foot nails Mr Howard Davies
16:15 Discussion Nikki Kelsall & Jayne Ward
16:25 Fibular nails are the answer to all our worries Tim White
16:35 There’s no problem with ORIF as a tried and tested method (& FAME) Xavier Griffin
16:45 Discussion Nikki Kelsall & Jayne Ward
16:50 Non-weight bearing post-op ankle fractures treats the surgeon not the patient Nigel Rossiter
17:00 How soon can an ankle fracture patient run Bob Carter
17:05 Discussion Nikki Kelsall & Jayne Ward
15:40 - 17:10 Advances in Osteoarthritis Research (BORS Revalidation)
This session chaired by BORS will provide four fascinating talks which provide an overview of current concepts and many of the latest developments in osteoarthritis research. We are proud to present 4 distinguished academic experts who will cover a breadth of topics.
Conference Suite 2A
Chaired by Wasim Khan
Co-Chaired by Salma Chaudhury
Agenda:
Epidemiology and Risk Factors for Osteoarthritis Mark Wilkinson
Advances in Cell Therapies for Osteoarthritis Cosimo de Bari
Advances in Bioengineering for Osteoarthritis Ruth Wilcox
Advances in Health Technologies for Arthritis Liba Sheeran
15:40 - 17:10 Management of early osteoarthritis and cartilage defects in the knee (BASK Revalidation)
The session will focus on the young patient with articular cartilage defects, including the use of osteotomy and stem cell therapies for osteoarthritis of the knee.
Conference Suite 2B
Chaired by Leela Biant
Speakers: Michael McNicholas, Professor Martyn Snow, Lesley Curwen and Professor Andrew McCaskie
Agenda:
Step by Step How to do a Safe HTO Live sawbone demonstration - Michael McNicholas
K Osteotomy Consensus Paper - Martyn Snow
The Stem Cell Hard Cell – UK Medical Journalist Prize Winner - Lesley Curwen (www.bbc.co.uk/programmes/m000cz1l)
Current evidence for stem cell therapies for OA of the knee - Andrew McCaskie
15:40 - 17:10 Infection/COVID-19 Free Papers
Conference Suite 3
Chaired by Rhidian Morgan-Jones and Tim Petheram
15:45 - 15:53 Pre-operative Biopsy has a higher sensitivity, specificity and likelihood of detecting a polymicrobial flora in Prosthetic Knee Joint Infection than aspiration alone - Patrick Hourigan
15:53 - 16:01 Outcomes after peri-operative SARS-CoV-2 infection in patients with proximal femoral fractures: an international cohort study - Chetan Khatri
16:01 - 16:09 IMPACT-Global: Prevalence, Clinical Predictors and Mortality Associated with COVID-19 in Hip Fracture Patients. An international multicentre study of 7,090 patients - Andrew Hall
16:09 - 16:17 Superior Tissue Levels of Vancomycin are Achieved with Intraosseous versus Intravenous Administration Despite Limited Tourniquet Use in Primary TKA: A Prospective, Randomized Trial - Henry Clarke
16:17 - 16:25 Cost-Effectiveness of Single versus Double DAIR with Antibiotic Beads for Acute Periprosthetic Joint Infections in TKA - Henry Clarke
16:25 - 16:33 The re-infection rate following 2 stage revision knee arthroplasty for peri-prosthetic joint infection: A retrospective review of 198 patients - Duncan Renton
16:33 - 16:41 Prosthetic Joint Infection (PJI) – Is this correctly recorded as a ‘Reason for Revision’ on the National Joint Registry? - Irrum Afzal
16:41 - 16:49 The Safe Resumption of Elective Orthopaedic Services following the first wave of the SARS-CoV-2 pandemic: a review of 2316 consecutive cases and implications for recovery following the current wave - Irrum Afzal
16:49 - 16:57 Long term follow-up adult long bone osteomyelitis managed with the modified Lautenbach procedure - Umar Yousuf
16:57 - 17:05 The Global Impact of COVID-19 on Surgeons and Team Members (Global COST) Study - Zahra Jaffry
17:20 - 18:50 Research for Optimising Orthopaedics (BOA Research Committee)
T&O clinical research is currently very healthy in the UK, with many trials ongoing and results from these filtering through to the clinic. So what are the latest findings and how could and should we all apply them? And how do we continue working to ensure a healthy pipeline of clinical research continues to benefit our current and future patients? Come to this session to hear more and join the debate!
Main Auditorium
Chaired by Hamish Simpson
Co-Chaired by Yuri Kulikov (1st half), Chinmay Gupte and Paul Baker (2nd half),
Speakers: Professor Sallie Lamb, Mike Whitehouse, Professor Alan Montgomery, Professor Dan Perry, Chloe Scott and Professor Xavier Griffin
Agenda:
17:20 - 18:00 - PART A: The past, present and future of T&O clinical research
Chairs: Professor Hamish Simpson, Yuri Kulikov and Chinmay Gupte
• Welcome and latest updates on BOA research activities: Professor Hamish Simpson
• Introducing the BOA-funded CTUs at Nottingham and Exeter: Professor Alan Montgomery (University of Nottingham) & Professor Sallie Lamb (University of Exeter)
• Keynote: The Evolution of Trauma and Orthopaedic Clinical Research: Professor Sallie Lamb
Profession Sallie Lamb is the Mireille Gillings Professor for Health Innovation and the Associate Dean of Research at the University of Exeter. She is an internationally recognised scholar in ageing, disability and rehabilitation. She is also an experienced methodologist in the area of clinical trials and high quality evaluation of health care practice. In particular, she strives to ensure research is translated into practice.
She has served as a Chair of the Health Technology Assessment Board and other senior roles in National Institute of Health Research and is a Trustee of the Versus Arthritis charity.
18:00 - 18:50 - Part B: Latest research that has or should change practice
Chairs: Professor Hamish Simpson, Paul Baker and Chinmay Gupte
• 1 stage or 2 stage Revision Hip Arthroplasty: Which Should I do?
The INFORM trial: Professor Mike Whitehouse, North Bristol NHS Trust & University of Bristol
• Which patients are suffering the most?
Worse than death: Chloe Scott, Royal Infirmary of Edinburgh & University of Edinburgh
Discussion Lead: Paul Baker
• Should we change how we treat children's forearm fractures?
The Force Trial: Professor Dan Perry, Alder Hey Hospital Liverpool & University of Liverpool
• How the WHiTE Trials have changed my Practice.
WHiTE trials 1-...: Professor Xavier Griffin, Barts and The London School of Medicine.
Discussion Lead: Chinmay Gupte
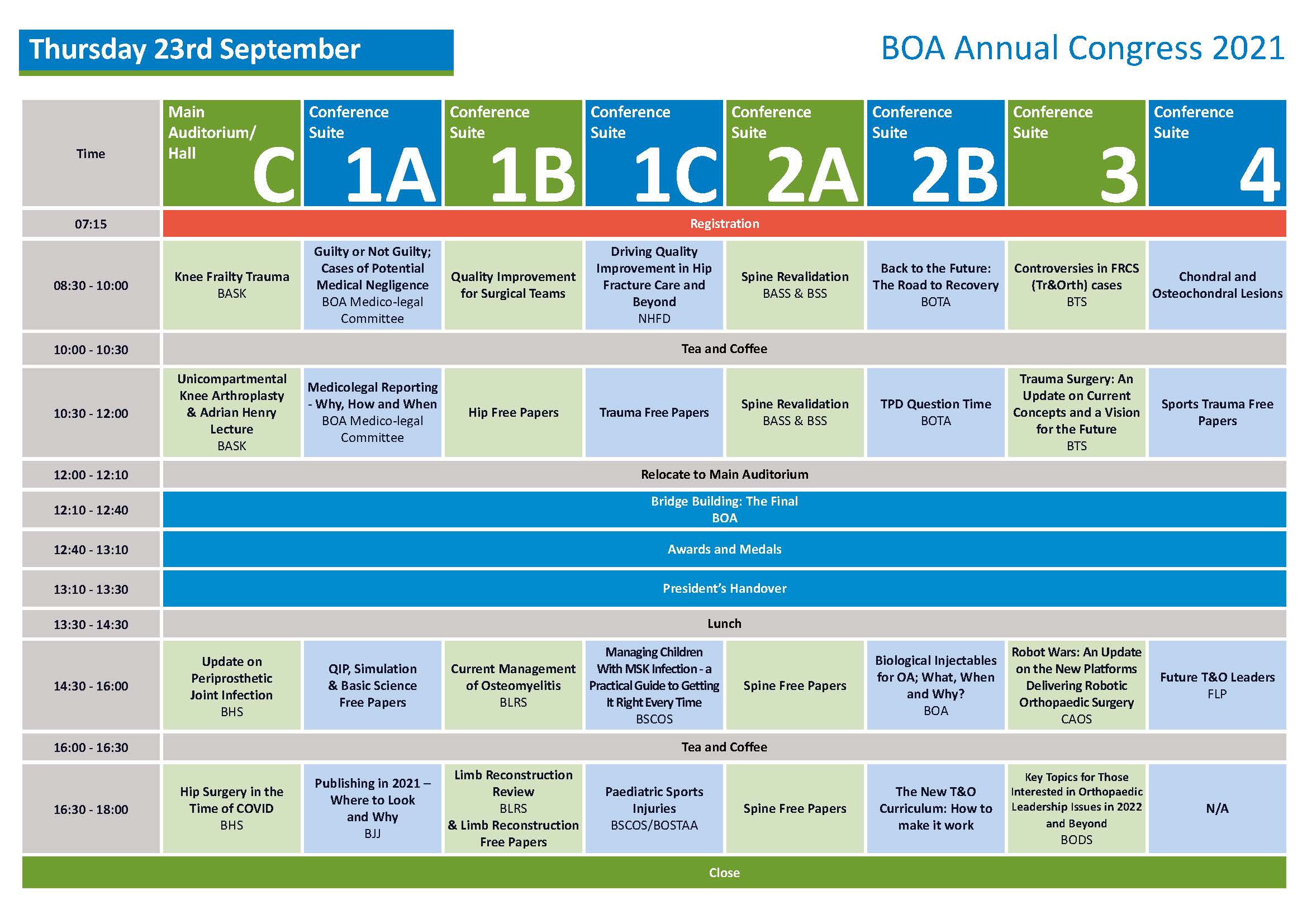
08:30 - 10:00 Knee Frailty Trauma (BASK Revalidation)
In this revalidation session we will look at trauma knee admissions with a focus on the frail patient. The talk will cover periprosthetic knee fractures, distal femoral fractures, proximal tibial fractures in the elderly including proximal tibial replacement.
Main Auditorium/Hall C
Chaired by James Murray
Speakers: Phil Hopgood, Alexander Dodds, Mike Kelly and Chloe Scott
08:30 - 10:00 Guilty or Not Guilty; Cases of Potential Medical Negligence
Orthopaedic surgeons who report regularly on cases of potential medical negligence will discuss marginal cases with a final comment from a barrister. The audience will have opportunities to ask questions and vote on the cases.
Conference Suite 1A
Chaired by Professor Grey Giddins
Speakers: Simon Britten and Simon Royston
08:30 - 10:00 Quality Improvement for Surgical Teams (QIST)
In this session we present and discuss the experience, results and learning from a cluster randomised controlled trial; Quality Improvement for Surgical Teams (QIST) – avoiding surgical site infection and anaemia at the time of surgery. The aim of which was to test the effectiveness of improvement collaboratives as a tool for introducing change at scale and pace in elective orthopaedics in the NHS.
Conference Suite 1B
Chaired by Professor Mike Reed
Co-Chaired by Gillian Davies
Speakers: Ashley Scrimshire, Sam Hook, Elizabeth Coleman, Dr Win Tadd, Dr Alwyn Kotze and Ajay Malviya
08:30 - 10.00 National Hip Fracture Database – Driving Quality Improvement in Hip Fracture Care and Beyond
This session will update the audience on hip fracture care across England, Wales and Northern Ireland. The impact of COVID on hip fracture care in 2020, the effect of best practice tariff over the years and potential future changes to incentivisation of excellent patient care will be presented and discussed. The new addition of non hip femoral fracture and periprosthetic femoral fracture data submission to the NHFD will also be discussed.
Conference Suite 1C
Chaired by Dominic Inman
Speakers: Professor Antony Johansen, Professor Matt Costa, Professor Xavier Griffin and Jonathan Evans
Agenda:
08:30 - 08:35 Welcome and Introduction to the session Dominic Inman
08:35 - 08:45 2020 – the COVID year from the perspective of hip fracture patients Professor Antony Johansen
08:45 - 09:00 WHITE – BPT, its effect on outcome following hip fracture and Quality standards used in other health systems Professor Matt Costa
09:00 - 09:10 REDUCE – a toolkit for hip fracture care Professor Xavier Griffin
09:10 - 09:20 Discussion
09:20 - 09:30 NHFD Key performance indicators – using the NHFD website to drive QI, and life after BPT? Professor Antony Johansen
09:30 - 09:40 Expansion of the NHFD – femoral shaft fractures and periprosthetic fractures Dominic Inman
09:40 - 09:50 Periprosthetic fractures – what we’ve learnt so far, what we need from you Jonathan Evans
09:50 - 10:00 Discussion
08:30 - 10:00 BASS/BSS Spine Revalidation
Conference Suite 2A
Chaired by Jayesh Trivedi
Speakers: Jayesh Trivedi, Andrew Frost and Rajat Verma
Agenda:
08:30 - 08:35 Introduction
08:35 - 08:50 Painful Spine in the child Jayesh Trivedi
08:55 - 09:10 Scoliosis and the orthopaedic Surgeon Jayesh Trivedi
09:15 - 09:30 Inflammatory Spine Conditions Andrew Frost
09:35 - 09:50 Diagnostic Dilemmas in Acute Spine conditions Rajat Verma
08:30 - 10:00 Back to the Future: The Road to Recovery (BOTA Revalidation)
Come join BOTA and our guest speakers as we reflect on T&O training throughout the COVID-19 pandemic and set out our vision for the road to recovery. We aim to deliver an insightful and engaging session that will give both Trainees and Trainers inspiration in the wake of the COVID-19 pandemic.
Conference Suite 2B
Chaired by Oliver Adebayo
Co-Chaired by Kriti Singhania
Speakers: Rob Gregory, Laura Deriu, Samantha Downie, Vicki Cherry and Uttam Shiralkar
Agenda:
• Lessons from the Trainer of the Year
• The New Curriculum Explained
• GOAST Study
• “Thrive not just Survive!”
08:30 - 10:00 Controversies in FRCS (Tr&Orth) cases (BTS Revalidation)
Eminent UK trauma surgeons discuss trauma cases and learning points especially for senior orthopaedic trainees.
Conference Suite 3
Chaired by Mr Ansar Mahmood
Speakers: Mr Tim White, Khitish Mohanty and Professor Benjamin Ollivere
Invigilator and referee: Mark Bowditch
08:30 - 10:00 Chondral and Osteochondral Lesions (BOSTAA Revalidation)
Chondral and osteochondral lesions represent a difficult treatment problem for the Sport’s Surgeon. There is no uniform approach to managing these patients. In this session we will explore the presentation and the different management options available. We will see how this problem affects various joints commonly affected by sport.
Conference Suite 4
Chaired by Professor Rhidian Thomas
Co-Chaired by Guido Geutjens
Agenda:
08:30 - 08:40 Diagnosis and assessment of chondral and osteochondral lesions Joanne Banks
08:40 - 08:50 Microfracture, Mosaicplasty or Allograft for the defect? Vipul Mandalia
08:50 - 09:00 Focal cartilage resurfacing Jon Smith
09:00 - 09:10 The multi-operated articular cartilage defect Andy Metcalfe
09:10 - 09:20 Discussion
09:20 - 09:30 Loose body in the adolescent’s knee. When to operate and the role of fixation Joanna Thomas
09:30 - 09:40 Talar dome lesions Carolyn Chadwick
09:40 - 09:50 Repetitive stress injuries in the elbow Adam Watts
09:50 - 10:00 Discussion
10:30 - 12:00 Unicompartmental Knee Arthroplasty (BASK Revalidation and Adrian Henry Lecture)
In this session we look at delivering a unicompartmental knee arthroplasty practice, including decision aids, training and starting a practice.
Main Auditorium/Hall C
Chaired by Andrew Price
Co-Chaired by Andrew Porteous
Speakers: Phil Hopgood and Daniël Saris
10:30 - 12:00 Medico-legal Reporting – Why, How and When
In this medico-legal session, we will find out whether there is a gender imbalance in medico-legal reporting. Then we will hear from 3 experienced medico-legal experts, all female, on how, when and why they run their medico-legal practices. An accomplished lawyer will tell us exactly what the legal profession do and don’t want to see in their medical experts. Finally, there will some tips on how to set up a medico-legal practice and how mentoring can help.
Conference Suite 1A
Chaired by Professor David Warwick
Co-Chaired by Sarah Johnson-Lynn
Speakers: Jacquelyn McMillan, Jan McCall, Simon Britten, Deborah Eastwood, Charlotte Lewis and Jo Round
Agenda:
10:30 - 10:40 Gender balance in medico-legal Reporting Jo Round
10:40 - 10:50 Why, how and when I run my medico-legal practice Charlotte Lewis
10:50 - 11:00 Why, how and when I run my medico-legal practice Deborah Eastwood
11:00 - 11:10 Why, how and when I run my medico-legal practice Jacqui MacMillan
11:10 - 11:20 What we lawyers do and don't like in a medico-legal expert Jan McCall
11:20 - 11:25 Setting up a medico-legal practice David Warwick
11:25 - 11:30 Mentoring in medico-legal reporting Simon Britten
11:30 - 12:00 Discussion
10:30 - 12:00 Hip Free Papers
Conference Suite 1B
Chaired by Simon Buckley & Henry Wynn-Jones
10:35 - 10:43 Long-term results of the original C-stem cemented polished triple-tapered femoral implant in a consecutive series of 500 cases: A 14 to 19 year follow-up study - David Sochart
10:43 - 10:51 Effect on health-related quality of life of the X-Bolt dynamic plating system versus the sliding hip screw for the fixation of trochanteric fractures of the hip in adults: the WHiTE Four randomised clinical trial - Xavier Griffin
10:51 - 10:59 Dual Mobility Cup Versus Conventional Total Hip Arthroplasty for Femoral Neck Fractures: An International Multi-Registry Study - James Masters
10:59 - 11:07 The Results: NIHR Feasibility RCT: Acetabular Fractures in older patients Intervention Trial (AceFIT: ISRCTN16739011). CI Andrew Carrothers, Joseph Alsousou, Daud Chou, Jaikirty Rawal, Joseph Queally, Peter HullAddenbrookes, Cambridge University Hospitals NHS Foundation Trust - Andrew Carrothers
11:07 - 11:15 Long-term survivorship of a flexible, titanium, HA coated, medium length revision stem. 140 cases at 10 years with the Corail® Revision Stem - Rohit Singhal
11:15 - 11:23 Defining the patient acceptable symptom state using the Forgotten Joint Score 12 following hip arthroscopy - Thomas Williamson
11:23 - 11:31 Managing the Interval in 2-Stage Revision for Prosthetic Joint Infection in Total Hip Replacement: Choice of Articulating Spacer? - James Coleman
11:31 - 11:39 Do post-operative hip precautions prevent dislocation following elective primary total hip arthroplasty? An analysis of a national administrative data set in England - John Machin
11:39 - 11:47 Surgeon experience with hip arthroplasty in severely obese patients reduces the risk of major complications; time for a referral network to be considered? - Alexander Charalambous
11:47 - 11:55 Cemented Charnley Total Hip Arthroplasty For Osteoarthritis Secondary To Developmental Dysplasia Of The Hip: 3-37 Years Follow Up Study - Samarth Arya
10:30 - 12:00 Trauma Free Papers (OTS / BTS)
Conference Suite 1C
Chaired by Mike Kelly
10:35 - 10:43 Fracture healing in patients with human immunodeficiency virus in South Africa: a prospective cohort study - Simon Graham
10:43 - 10:51 Manipulation of Distal Radius Fractures: A Comparison of Bier’s block Vs Haematoma block - Ben Oakley
10:51 - 10:59 Timing of surgery for internal fixation of intracapsular hip fractures and complication at 1 year; a 35-year clinical study of 2366 patients at a single Level 2 trauma centre - Senthooran Kanthasamy
10:59 - 11:07 Identifying Research Priorities in Musculoskeletal Trauma Care in Sub-Saharan Africa - Simon Graham
11:07 - 11:15 Ankle Injury Rehabilitation (AIR): a multicentre randomised controlled trial and economic evaluation - Rebecca Kearney
11:15 - 11:23 Exposing the incidence of ileus in pelvic and acetabular fractures: a retrospective case analysis - Janine Adedeji
11:23 - 11:31 Surgical treatment of dorsally displaced distal radius fractures with a volar locking plate versus conventional percutaneous methods: minimum ten-year follow-up of a randomised controlled trial - Sandeep Deshmukh
11:31 - 11:39 Implications of a Specialist Hip Fracture Service on Outcomes after Internal Fixation of a Trochanteric Hip Fracture - Alexandra Macmillan
11:39 - 11:47 Hindfoot Ankle Reconstruction Nail Trial (HARNT) - A National collaborative study of complex ankle fractures in the United Kingdom - Caesar Wek
11:47 - 11:55 Factors Associated with Long-term Outcome Following a Humeral Shaft Fracture: Results for 291 Patients at a Minimum One-Year Follow-Up - William Oliver
10:30 - 12:00 BASS/BSS Spine Revalidation
Conference Suite 2A
Chaired by Santosh Baliga
Speakers: Santosh Baliga, James Walkden, Pragnesh Bhatt and Peter Bodkin
Agenda:
10:30 - 10:45 Immediate assessment, care and referral of spinal trauma Santosh Baliga
10:50 - 11:05 Spinal Infection James Walkden
11:20 - 11:35 Cauda Equina Syndrome Pragnesh Bhatt
11:40 - 11:55 Metastatic Spinal Cord Compression Peter Bodkin
10:30 - 12:00 TPD Question Time (BOTA)
Don't miss out on your chance to get your burning questions on T&O training after COVID-19 answered. Join BOTA as we welcome TPDs and the SAC chair to the stage, where they attempt to tackle the most topical and challenging questions submitted by Trainees and Trainers across the UK. Audience participation will be encouraged and we will ensure that no stone is left unturned.
Conference Suite 2B
Chaired by Rob Gregory
Co-Chaired by Graham Finlayson
Speakers: Donald Campbell & Oliver Adebayo
10.30 - 12.00 Trauma surgery: An update on current concepts and a vision for the future (BTS Revalidation)
Three expert speakers will give an update on current concepts and potential for future developments.
Conference Suite 3
Chair by Professor Alan Johnstone
Speakers: Professor Peter Giannoudis, Professor Alan Johnstone and Ansar Mahmood
Agenda:
Masquelet technique: What have we learned? Professor Peter Giannoudis
Current concepts update on extremity compartment syndrome Professor Alan Johnstone
Artifical Intelligence in Trauma Ansar Mahmood
10:30 - 12:00 BOSTAA Free Papers (Shoulder and Elbow Instability Revalidation)
Conference Suite 4
Chaired by Nick Nicolaou and Neil Jain
Speakers: Ben Gooding and Kapil Kumar
Agenda:
Free Papers - Sports Trauma (45 minutes)
10:35 - 10:43 Positive predictors of a good outcome following surgical fasciotomies for chronic exertional compartment syndrome (CECS) and a predictive scoring system to guide management - Christopher Trew
10:43 - 10:51 Return to Competition Following Clavicle Fractures in Professional Road Cyclists - Matthew Walmsley
10:51 - 10:59 Strength and proprioception are preserved following internal brace repair of the anterior cruciate ligament - William Wilson
10:59 - 11:07 Factors Associated with Return to Work and Sport following a Humeral Shaft Fracture - William Oliver
Shoulder Instability in athletes Kapil Kumar (20 minutes)
Elbow Instability in athletes Ben Gooding (20 minutes)
12:10 - 12:40 BOA Plenary - The Bridge Final
Bridge Building - The Final.
See which team's bridge passes the weight bearing test with Oliver Budd.
The 4 teams:
The British Orthopaedic Trainees Association BOTA
The Future Leaders Programme FLP
The British Hip Society BHS
The Orthopaedic Trauma Society OTS
12:40 - 13:10 Awards and Medals
13:10 - 13:30 President's Handover
14:30 - 16:00 Update on Periprosthetic Joint Infection (BHS Revalidation)
This session will update delegates knowledge of the current treatment of PJI in hip arthroplasty. This is based on the recently published BOAST and will cover presentation, investigation and treatment options.
Main Auditorium/Hall C
Chaired by Professor Dominic Meek
Speakers: Richard Westerman, Jason Webb, Tim Petheram and Paddy Ashcroft
PJI setting the scene Dominic Meek
MDT structure Tim Petheram
Clinical Presentation & Diagnosis Jason Webb
DAIR Richard Westerman
Revision surgery options for PJI Paddy Ashcroft
Case Discussions All
14:30 - 16:00 QIP, Simulation & Basic Science Free Papers
Conference Suite 1A
Chaired by Simon Hodkinson
14:43 - 14:51 Total hip arthroplasty - The Consequences of Not Templating - Benjamin Kapur
14:51 - 14:59 Real time measurement of intramuscular pH during routine knee arthroscopy and arthroplasty using a tourniquet: A preliminary study - David MacDonald
14:59 - 15:07 Use of a Blast Wave Represents a Novel Therapy for Enhancing the Osteogenic Capacity of Mesenchymal Stem Cells - Sarah Stewart
15:07 - 15:15 National Joint Registry recorded untoward intraoperative events during primary total hip arthroplasty: An investigation into the data accuracy, causal mechanisms and attributability - Rohit Singhal
15:15 - 15:23 Introduction of an Intranasal Diamorphine pathway for manipulation of paediatric forearm and distal radius fractures in the Emergency Department - Tomos Richards
15:23 - 15:31 Improving Humeral Shaft Fracture Management: Implementation of a new clinical pathway - Joanne McKay
15:31 - 15:39 Service development in response to Coronavirus Pandemic: Setting up the Aberdeen Virtual Hand Service - Katharine Hamlin
15:39 - 15:47 Hip fracture surgery performed by cadaveric simulation-trained versus standard-trained residents: a pragmatic multicentre randomised controlled trial - Hannah James
14:30 - 16:00 Current Management of Osteomyelitis (BLRS Revalidation)
An update in surgical decision making, investigation and management strategy in chronic osteomyelitis and fracture related infection.
Conference Suite 1B
Chaired by Peter Calder
Co-Chaired by Amir Qureshi
Speakers: Hemant Sharma, Professor Martin McNally, Dr Zia Saad, Dr Kordo Saeed, Nima Heidari and Om Lahoti
Agenda:
14:30 - 14:35 Introduction Hemant Sharma
14:35 - 15:10 Evolution Not Revolution in Managing Bone Infection Professor Martin McNally
15:10 - 15:20 Diagnostic Update: Beyond Hot Spots – Nuclear Medicine & Molecular Imaging Innovations in MSK Infection Diagnostics Dr Zia Saad
15:20 - 15:30 Diagnostic Update: Phage Therapy, What is on the Horizon for MSK Infections? Dr Kordo Saeed
15:30 - 15:55 Fracture Related Infection Update Nima Heidari
15:55 - 16:00 Closing Remarks Om Lahoti
14:30 -16:00 Managing Children with MSK Infection- a practical guide to getting it right every time (BSCOS Revalidation)
Paediatric musculoskeletal infection remains one of the core time-critical emergencies that every orthopaedic surgeon on-call should be able to manage competently. Yet, the spectrum of diagnoses and the varied presentation make for uncertainty and trepidation in those who are inexperienced, and even more so in those with experience. What tests? What scans? When is an operation required? Which cases should be managed in specialist centres? This session aims to clear up some of the confusion and provide clarity. An interactive discussion of several different cases with an expert panel will provide food for thought and learning points to take home and incorporate into practice. Consensus guidelines for the management of MSK infection in children have been produced by BSCOS, and will be shared and explained in this session. And how should specialist and non-specialist centres work together to ensure high quality care for every child within a region? We’ll hear from one of the most recently established regional networks specifically created to ensure every child gets the care they need 24/7.
Conference Suite 1C
Chaired by Anish P Sanghrajka
Co-Chaired by Nigel Kiely
Speakers: Clare Carpenter, Philip Henman, Piers Mitchell and Helen Chase
Agenda:
14:30 - 15.15 Managing the child with suspected MSK infection: Interactive Case discussions Clare Carpenter, Philip Henman and Anish Sanghrajka
15:15 - 15:45 New national consensus guidelines for the management of paediatric MSK infection Piers Mitchell
15:45 - 16:00 Regional networks for the management of paediatric MSK infection Helen Chase
To participate in live polls and view results, access Vevox from your web browser: https://vevox.app/#/m/185404417 Or enter Session ID: 185-404-417 in the Vevox app.
14:30 - 16:00 Spines Free Papers
Conference Suite 2A
Chaired by Rohit Shetty
Co-Chaired by James Tomlinson
14:30 Cervical Myelopathy Rohit Shetty
Free Papers:
14:50 - 14:57 Long Term Core Outcomes in Cauda Equina Syndrome - Thomas Barker
14:57 - 15:04 Impact of a local pathway on the waiting time for MRI in patients presenting to a district general hospital with suspected cauda equina syndrome - Hossam Fraig
15:04 - 15:11 The Effects of the Covid-19 Pandemic on Cauda Equina Syndrome Referrals in the Scottish Highlands - Luliana Kanya
15:11 - 15:18 Mortality predictors for operative management of acute sub-axial cervical spine fractures in elderly patients - Abdul Azeem Badurudeen
15:18 - 15:25 Routine in-hospital radiographs following anterior cervical discectomy and fusion surgery: neither necessary nor cost-effective? - Rory Michael McCabe
15:25 - 15:32 Fusion and Subsidence in Cervical Disc Replacements - A Retrospective Cohort Study - Oliver Beaumont
15:32 - 15:39 Assessing the Validity Of A Temperature Sensor To Monitor Patient Adherence To Cervical Spine Orthosis Wear Time - Elizabeth Headon
15:39 - 15:46 Decompression alone versus decompression with fusion for treatment of degenerative spinal foraminal stenosis: A systematic review - Pratik Shah
15:46 - 15:53 The effects of long-term blood thinner usage on the operative complications and patient-reported outcome measures of elective lumbar microdecompression surgery - Madhumita Kolluri
14:30 - 16:00 Biological injectables for OA; What, when and why?
The concept of biological joint regeneration is hugely attractive to patients and to the medical community. We have strived for many years to look at options to repair or replace articular cartilage and maintain joint function in order to allow patients to continue pain-free activity and to avoid the consequences of osteoarthritis and its associated symptoms and the ultimate need for joint arthroplasty.
Whilst there has been tremendous progress and development in the joint arthroplasty field, research into regenerative therapies has been slower to translate to the bedside. There is, however, renewed interest, and a global industry valued at over £5 billion looking at joint preservation through biological means. There is some concern that indiscriminate use of these approaches may undermine targeted clinical use and legitimate clinical research.
While we very much hope that this will be part of the long-term solution to joint injuries and joint degeneration, considerable debate remains over which strategies to use, their mechanism of action, and their potential short and long term effects on patients. There are important considerations in relation to unvalidated treatments, uncontrolled marketing, short term symptomatic control and the possibility of long term regenerative effects. We are now at a critical stage where we really need to consider the strategies are available to us and how they should be regulated and used in clinical practice.
This symposium will cover the current dilemmas in this area and the options available and will assess the available peer reviewed literature. We will explore the most appropriate means for reporting and evaluating these interventions, consider how best to educate patients and surgeons on emerging research evidence, and discuss potential future challenges and regulatory frameworks.
There is great controversy in this area. The holy grail of biological joint restoration remains integral to orthopaedic thinking. We must for now however agree systems for the evaluation, the reporting, the translation and the regulation of biological therapies for joint arthritis.
Conference Suite 2B
Chaired by Mark Bowditch
Co-Chaired by Fares Haddad and Caroline Hing
Speakers: Andrew McCaskie, Connie Chu, Iain Murray, Ansar Mahmood and Ian Rees
Agenda:
Welcome Mark Bowditch
Introduction and setting the scene Fares Haddad (5 minutes)
Reporting guidelines for valid research Iain Murray (10 minutes)
Point of care manufacturing and regulatory considerations Ian Rees, MHRA (5 - 10 minutes)
What surgeons and patients need to know Andrew McCaskie (15 minutes)
Biological injections in OA – state of the art and future strategies Connie Chu (pre-recorded 15minutes)
Fat and Bone Marrow based point of care injections now: When/Why/Where? Ansar Mahmood (15 minutes)
Questions and case discussions Caroline Hing/Mark Bowditch (20 minutes)
Sum up Fares Haddad
Close Mark Bowditch
14:30 - 16:00 Robot Wars - An update on the new platforms delivering Robotic Orthopaedic Surgery (CAOS Revalidation)
In the mid-nineties, orthopaedic surgeons mainly driven by spine and joint replacements surgeons introduced computer assisted and robotic devices into their practice with the potential to reduce outliers in surgical practice and ultimately improve outcomes and reduce short and long-term complications and revisions.
Three main classes of devices were conceived and developed over the years to achieve these goals: there were the navigation systems, the patient-specific instruments (PSI) and the robotic devices. All three used either pre-operative planning issued from patient specific medical imaging (MRI or CT scan) or only intra operative anatomic data collection or “image free guidance”. All three aimed to assist the surgeons intraoperatively. Navigation and robotic systems both adopt user-interfaces depicting simultaneously the pre/intraoperative plan and tracked instruments to perform the surgery. PSI uses preoperative planning and manufactured guides to fit the patient’s anatomy to perform the surgery. Robotic technology relies on similar concepts implemented in navigation, but the final surgical action is either performed or guided by a robotic arm or hand held smart device (Active or controlled robotic technology) instead of only the surgeon.
Computer assisted and robotic technology has been used all over the world for more than 25 years with variable success but is not yet mainstream standard of care and is only used by a limited number of surgeons. The technology has confirmed its benefits in improving the accuracy and precision of the surgery and clinical evidence is growing to support the implementation of these systems in everyday practice.
Orthopaedic implant companies have invested heavily in the development of these new technologies as evidenced by the recent growth in robotic technology, developing different systems in design and execution. The goal of this session is to present these devices in the most clinically objective way for the audience to understand how they work and what they can expect from their use-the faculty are taken from leading UK and International clinicians who are involved in their development and use the systems regularly.
It is undeniable that computer and robotic technology has invaded all workplaces and has demonstrated its efficiency. The orthopaedic speciality won’t escape this new paradigm. However, it is still difficult to identify not only the long-term benefits of these new “tool-boxes” but also the real differences between all these systems. We hope to discuss some of these issues during the course of this session.
Conference Suite 3
Chaired by Dinesh Nathwani, Frédéric Picard & Ajeya Adhikari (chair & speaker)
Speakers: Professor Ferdinando Rodriguez y Baena, Professor Andrew Toms and Kamal Deep
Agenda:
14:30 - 14:35 Introduction Dinesh Nathwani (CAOS UK President)
14:35 - 14:48 Introduction to Robotics in Orthopaedics: Background and overview from an engineering perspective Professor Ferdinando Rodriguez y Baena
14:48 - 15:00 Image based robotic arm assisted arthroplasty - the evidence is growing Professor Andrew Toms
15:00 - 15:12 Hand-held image free robotic knee replacement - the introduction of Personalised hybrid Alignment Dinesh Nathwani
15:12 - 15:24 Robotics versus navigation in hip replacement Kamal Deep
15:24 - 15:36 Clinical overview of the Robotic Surgical Assistant (ROSA®) Akash Sharma
15:40 - 16:00 Q&A Roundtable discussion Chair: Frédéric Picard / Ajeya Adhikari
14:30 - 16:00 Future T&O Leaders (FLP)
Today’s NHS demands innovative, creative, adept, reflective, experiential leaders to deal with the complex and unpredictable world of healthcare. Our leaders need to be able to see the bigger picture, manage risk and be able to cope with solving problems resulting from increased longevity with chronic disease burden and the social pressures of unemployment and poverty· This session is aimed at leaders and potential leaders at every level of the organisation: from trainees through to established consultants and leaders. Leadership has been fully integrated into our T&O curriculum through Generic Professional Capabilities and Capabilities in Practice. But the real need to integrate leadership training goes well beyond such rules and regulations.
Conference Suite 4
Chaired by Hiro Tanaka
Co-Chaired by Lisa Hadfield-Law
Speakers: Pramod Achan, Andrea Sott and Professor Tim Briggs
Agenda:
14:30 - 14:40 Introduction Hiro Tanaka
14:40 - 14:55 National Director of Clinical Improvement for the NHS & NHSI Professor Tim Briggs
- Tips and tricks on how to scale up QI at a national level
- How he came up with the GIRFT idea and then took it national
14:55 - 15:10 Interview with Pramod Achan
- What leadership development is available and feasible?
- What do you need as a trainee to meet leadership requirements?
- What do trainers need to train for leadership?
15:10 - 15:25 Interview with Andrea Sott
- What would you have done differently as a leader?
- What were the lessons you’ve learned?
- How have you done it?
15:40 - 15:55 Q&A
15:55 - 16:00 Summary
16:30 - 18:00 Hip Surgery in the Time of COVID (BHS Revalidation)
This session will explore the challenges facing hip surgery in the presence of endemic Covid-19, from patient consent, the practicalities of surgery, risk management and training.
Main Auditorium/Hall C
Chaired by Simon Buckley
Speakers: Chloe Scott, Tim Board, Ajay Malviya, Andrew Hamer, Andrew Gordon and Rob Gregory
Agenda:
Waiting is worth than death Chloe Scott
REJOIN study. Is it safe to operate? Tim Board
NAHR study of COVID safety and patient outcomes Ajay Malviya
Prioritisation for surgery, a National picture Andrew Hamer
Strategies to support patient waiting Andrew Gordon
Training under pressure Rob Gregory
Questions and Discussion
16:30 - 18:00 Publishing in 2021 – Where to Look and Why (BJJ)
This session will give an overview of Publishing in 2021 and an insight into the considerations authors and reviewers should have when approaching a manuscript. We will provide practical guidance on how to get funding for research, how to setup a trial properly as well as how to write a good paper. We will also cover how to maximise engagement after publication and setting up a journal club.
Conference Suite 1A
Chaired by Professor Fares Haddad
Co-Chaired by Elizabeth Ashby
Speakers: Elizabeth Ashby, Professor Daniel Perry, Professor Duncan Tennent, Professor Matt Costa and Chloe Scott
Agenda:
Introduction Professor Fares Haddad
Trials and evidence synthesis Professor Matt Costa
Research funding and collaboration Professor Dan Perry
What should you be reading to guide your practice Elizabeth Ashby
How to write a good paper Professor Duncan Tennent
Maximising engagement after publication Chloe Scott
Discussion
16:30 - 18:00 Limb Reconstruction Review and Free Paper Session (BLRS)
An update on what is new in Limb Reconstruction followed by a free paper session
Conference Suite 1B
Chaired by Peter Calder
Co-Chaired by Amir Qureshi
Speakers: Bilal Jamal, Louise McMenemy, Thomas Donnelly, Deborah Eastwood, Peter Calder, Khalid Al-Hourani, Muhammad Adeel Akhtar, Ganesh Mohrir, Mark Robinson and Chichi Menakaya
Agenda:
16:30 - 16:50 What’s New in Limb Reconstruction? Bilal Jamal
16:50 - 18:00 Free Paper Session (9 papers)
16:55 - 17:02 Limb salvage surgery: Progress since the Lower Extremity Assessment Project (LEAP) – a systematic review of the literature - Louise McMenemy
17:02 - 17:09 Complex Ankle arthrodesis with a circular frame: A prospective multicentre cohort study showing 100% union rates and complete deformity correction - Thomas Donnelly
17:09 - 17:16 Tension band plating for the correction of leg length discrepancy - Deborah Eastwood
17:16 - 17:23 Management of severe congenital deficiency of the femur: Has much changed in the 21st Century? - George Cross
17:23 - 17:30 Femoral offset angle: Correction of congenital distributed (multi-apical) deformity of the femur utilizing a novel technique - Khalid Al-Hourani
17:30 - 17:37 Osseointegration for Transtibial Amputees Confers Mobility Benefits with Limited Complications through Two Years - Muhammad Adeel Akhtar
17:37 - 17:44 Tibial Bone Defects: Analysis Of Time To Union And Direct Medical Costs Using Distraction Osteogenesis With An Ilizarov Frame Or The Masquelet Technique - Ganesh Mohrir
17:44 - 17:51 A Multi-centre 10-year Review of Elderly, Osteoporotic and Low Energy Schatzker V and VI Injuries managed with Ilizarov Circular Frame Constructs in Northern Ireland - Mark Robinson
17:51 - 17:58 Achieving Distal Fixation and Early Mobilisation In Patients with Severe Femoral Bone Loss Using an Internal Proximal Femoral Replacement Prosthesis Chichi Menakaya
16:30 - 18:00 Paediatric Sports Injuries (BSCOS/BOSTAA Revalidation)
An interactive session discussing sports injuries in the child and adolescent age group. A combined session between the British Society for Children's Orthopaedics (BSCOS) and the British Orthopaedic Sports Trauma and Arthroscopy Society (BOSTAA).
Conference Suite 1C
Chaired by Emily Baird
Co-Chaired by Nick Nicolaou
Speakers: Fazal Ali, David Hollinghurst, Chinmay Gupte, Hywel Davies, Nev Davies, Virginie Pollet and Rachel Hutchinson
Agenda:
16:30 - 17:10 Overview of Paediatric ACL Reconstruction Fazal Ali
Interactive Case Discussions - ACL reconstruction Moderator Nick Nicolaou
David Hollinghurst; Chinmay Gupte; Hywel Davies
17:10 - 17:30 Current Concepts in Paediatric Injury Prevention Nev Davies
17:30 - 18:00 The Paediatric Athlete with disability Moderator - Emily Baird
Introduction and overview Virginie Pollet
Clinical Cases Rachel Hutchinson
Discussion
16:30 - 18:00 Spines Free Papers
Conference Suite 2A
Chaired by Rohit Shetty
Co-Chaired by James Tomlinson
16:35 - 16:42 Comparative Study of PELD Percutaneous Endoscopic Lumbar Discectomy versus Traditional Surgical Discectomy Treatment Lumbar Disc Herniation - Ahmed Alkhuzai
16:42 - 16:49 Preoperative neutrophil-lymphocyte ratio (NLR) and lymphocyte percentage are useful predictors of postoperative complications after lumbar fusion - Temidayo Osunronbi
16:49 - 16:56 Standardising post-operative care documentation in spinal surgery through a simple, innovative, quality improvement process - Callum Edmonds
16:56 - 17:03 Pedicle Screw Insertion - an Educational Assessment of Accelerated Learning - Bisola Ajayi
17:03 - 17:10 The impact of the COVID-19 pandemic first national lockdown on emergency referrals to a tertiary referral spine centre - Daniel Tadross
17:10 - 17:17 Comparison of SPECT/CT with MRI in imaging scoliosis: Does SPECT/CT provide superior diagnostic information? - Daniel Thurston
17:17 - 17:24 Histopathological and Microbiological assessment of Paraspinal muscle tissue following spine surgery at a tertiary care centre - Sudeep Date
17:24 - 17:31 Creation of an Osteoporotic Vertebral Fracture Pathway - Louis Hainsworth
17:31 - 17:38 Optimisation and validation of a new low profile adherence sensor for monitoring spinal orthosis wear-time - Dominic Wardell
17:38 - 17:45 Consent Is a Process Not Just a Form - Olivia Payton
16:30 - 18:00 The New T&O Curriculum: How to make it work
The new curriculum has now been launched and the preparation of the last couple of years is being put into practice. This session aims to summarise what is required of the orthopaedic trainer and will focus on areas that may appear unclear, contentious or challenging with ample opportunity to answer any queries relating to implementation.
Conference Suite 2B
Chaired by Lisa Hadfield-Law, Rob Gregory
Speakers: Deepa Bose and Donald Campbell
Agenda:
What does the new curriculum actually mean for me as a trainer? Rob Gregory (5 minutes)
What have we learned about the MCR from V-TOES? Lisa Hadfield-Law (10 minutes)
How can we all make life easier for the TPDs? Donald Campbell (5 minutes)
How do we manage trainees who remain on the old curriculum? Deepa Bose (5 minutes)
Themed Q&A session (35 minutes with option to extend by 30 minutes):
a) Setting aside time for the MCR.
b) Managing colleagues who won't engage.
c) The relationship between the MCR and the ARCP.
d) Understanding how many WBAs will be needed.
e) Other questions.
16:30 - 18:00 Key topics for those interested in orthopaedic leadership issues in 2022 and beyond - British Orthopaedic Directors Society (BODS)
All Congress delegates welcome
Conference Suite 3
Chaired by Mike Reed
Co-chaired by Alan Middleton and Ajit Shetty
Speakers: Ananda Nanu, Bibhas Roy, Professor Sir Norman Williams, Marina Bogovac, Martin Campbell and Julian Owen
Agenda:
Welcome Mike Reed
Section Chair: Alan Middleton
Annualised job plans should be used in preference to traditional job plans Ananda Nanu v Bibhas Roy (30 minutes)
Section Chair: Mike Reed
The National Consultant Information Programme (NCIP) – GIRFT data at surgeon level Professor Sir Norman Williams and Marina Bogovac (20 minutes plus questions)
Section Chair: Ajit Shetty
How the money flows in the new world Martin Campbell, NHSEI (25 minutes)
Audience discussion + 5 minutes for questions)
BODS regions Julian Owen (5 minutes)
Close Mike Reed
Pre-recorded - ATOCP/Physiotherapy QI and Research Presentations
Chaired by Anthony Gilbert
Video introduction to session:
A Pre-recorded video link for the session presentations will be shared on Thursday 23rd September and is available to Congress ticket holders here.
Agenda:
QI presentations:
Pre-op triage system for elective non weight bearing foot and ankle patients to aid day of surgery discharge and prevent prolonged inpatient stays Hayley Price and Natalie Gofton
Introduction of a Daycase Total Hip Replacement Service Karen Barker and Simon Newman
Enhanced Recovery in Arthroplasty Katrina Mitchell
Research Presentations:
Development of a Virtual Knee School Anna Anderson
Brachial plexus injury: Living with uncertainty Caroline Miller
Can a brief behavioural assessment and tailored exercise adherence strategies improve adherence to exercise for older people with musculoskeletal conditions? A feasibility randomised controlled trial Jon Room
Pre-recorded - ATOCP/Physiotherapy Free Papers
Chaired by Anthony Gilbert
Video introduction to session:
A Pre-recorded video link for the session presentations will be shared on Thursday 23rd September and is available to Congress ticket holders here.
Therapy contributions to a systemic rapid recovery change programme in elective orthopaedics - Alexa Coyle
Does hip dislocation increase with the cessation of hip precautions following elective primary total hip arthroplasty? - Rene Gray
Is the deep squat test a valid and reliable test for the diagnosis of femoral acetabular impingement? A systematic review - Simon Wood
Physiotherapy Process Benchmarking: Analysis of Current Practice - Katherine Hodson
Survey: Are Hip Precautions Necessary on Discharge Following Hemiarthroplasty for Neck of Femur Fractures? - Sundas Butt
Do baseline scores or comorbidities affect patient-reported outcome measures following first metatarsophalangeal joint arthrodesis? - Vidhi Adukia
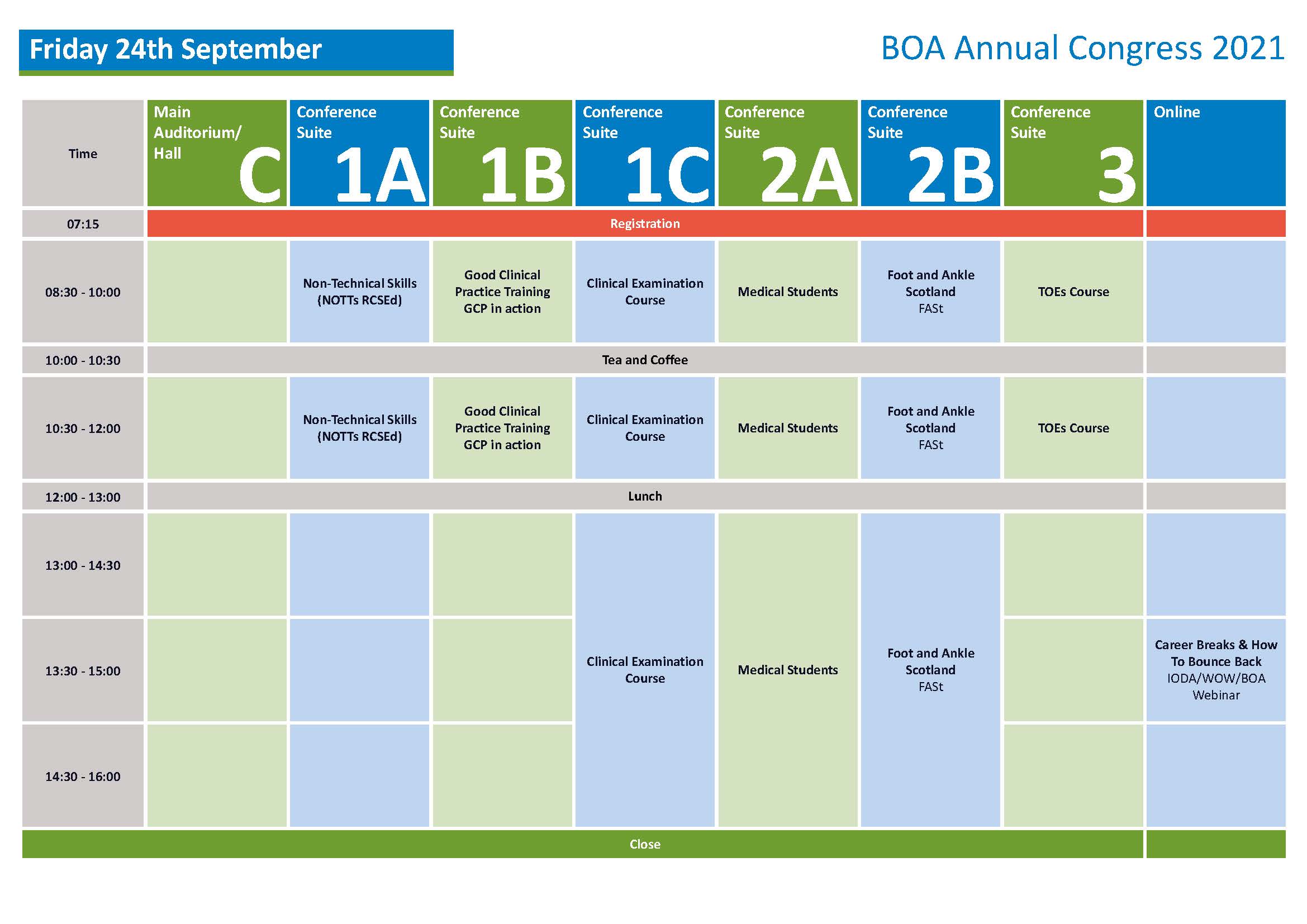
08:30 - 12:00 Non-Technical Skills for Surgeons (NOTSS)
The aim of the NOTSS project was to develop and test an educational system for assessment and training of non-technical skills in the intra-operative phase of surgery. NOTSS is a behaviour rating system based on a skills taxonomy that allows valid and reliable observation and assessment of four categories of surgeons' non-technical skill: situation awareness, decision making, communication & teamwork, and leadership.
These are the essential non-technical skills surgeons need to perform safely in the operating room and NOTSS allows measurement of several ACGME (Accreditation Council for Graduate Medical Education) competencies, including professionalism, interpersonal and communication skills, and systems-based practice. The skills taxonomy can be used to structure training and assessment in this important area of surgical competence.
Conference Suite 1A
Chaired by Nigel Kiely
Co-Chaired by James Tomlinson
08:30 - 12:00 Good Clinical Practice Training, GCP in Action
This session will describe the purpose of Good Clinical Practice (GCP) and outline the significant milestones in the history of GCP development. It will look at the impact of ICH GCP changes on investigator sites and sponsors. The current legislation relating to clinical trials and medical devices will be discussed. The practical application of GCP will be reviewed.
Conference Suite 1B
Chaired by Sue Fitzpatrick
08:30 - 10:00
- Welcome and Introduction
- History and purpose of GCP
- Development of ICH GCP
- Roles and responsibilities in clinical research according to ICH GCP
~Sponsor
~Monitor
~Investigator
~Ethics Committees
- ICH GCP E6 R2
- Changes in Data Protection with GDPR
- The EU Clinical Trial Regulation 536/2014, Directive 2001/20/EC and GCP Directive 2005/28/EC in addition the Directive 93/42/EEC on medical devices (EU MDD) Directive 90/385/EEC on active implantable medical devices (EU AIMDD) Directive 98/79/EC on in vitro diagnostic medical devices (EU IVDD) and current position
- The UK Statutory Instruments
10:00 - 10:30 Break
10:30 - 12:00
- GCP in action
- Essential Documentation
- Maintaining data integrity
- Informed consent
- Safety reporting
- Drug accountability
- Enforcement procedures
On completion of the session a GCP certificate will be awarded.
08:30 - 16:00 BOA Clinical Examination Skills Course
The BOA Clinical Examination Course was set up almost a decade ago with the aim that trainees will attend on an annual basis whereby skills could be learnt at an early stage of training and repetition would result in perfecting a technique and consequently improvement in patient care and examination success.
It is taught by an experienced group of lecturers on clinical examination techniques. The format includes a morning of lectures covering all regions of the body. This is followed in the afternoon by a hands-on session where participants rotate in groups of similar skill level. In these tutorial groups there is a demonstration by an experienced consultant followed by practice in pairs of the techniques learnt.
The feedback in previous years of this format of learning has been exceptional.
Conference Suite 1C
Chaired by Fazal Ali
Co-Chaired by Karen Robinson
Agenda:
08:00 - 08:30 Registration
08:30 - 08:50 Examination of the Hip Paul Banaszkiewicz
08:50 - 09:10 Examination of the Knee Paul Haslam
09:10 - 09:30 Examination of the Foot and Ankle Yulanda Myint
09:30 - 10:00 Examination of the Spine Alex Baker
10:00 - 10:30 Coffee
10:30 - 10:50 Examination of the Shoulder Ben Gooding
10:50 - 11:05 Examination of the Elbow Amjid Ali
11:05 - 11:30 Examination of the Hand Joe Garcia
11:30 - 12:45 Lunch
12:45 - 15:45 Practical Stations
Participants rotate in groups (based on experience) through stations every 20 mins. ALL FACULTY
Station
Hip — Holloway, Thiagarajah (Fernandes)
Knee — Chandrasenan, Quah (Haslam)
Foot & ankle — Obakponovwe, Myint (Lasrado)
Spine — Jain, Isaacson (Baker)
Shoulder — Gooding, MacInnes (Shahane)
Elbow — Booker, Sinha (A Ali)
Hand — Azhar, Gillott (Garcia)
Peripheral nerve — Robinson, Blakey (Wembridge)
Spare/Circulating — F Ali, Banaszkiewicz
16:00 CLOSE
Faculty:
Fazal Ali - Convener (Chesterfield)
Karen Robinson- Convener (Sheffield)
Joe Garcia (Chesterfield)
Shantanu Shahane (Chesterfield)
Jeevan Chandrasenan (Chesterfield)
Amjid Ali (Sheffield)
James Fernandes (Sheffield)
Paul Haslam (Doncaster)
Paul Banaszkiewicz (Gateshead)
Simon Booker (Sheffield)
Irwin Lasrado (Portsmouth)
Caroline Blakey (Sheffield)
Kevin Wembridge (Rotherham)
Ben Gooding (Nottingham)
Alex Baker (Preston)
Antonia Isaacson (Newcastle)
Scott McInnes (Doncaster)
Azhar Armughan (Lincoln)
Ed Holloway (Chesterfield)
Yulanda Myint (Nottingham)
Oghor Obakponovwe (Chichester)
Shankar Thiagarajah (Doncaster)
Apurv Sinha (Chesterfield)
Elizabeth Gillott (Derby)
Conal Quah (Derby)
Aanchal Jain (London)
08:30 - 16:00 Medical Students
This session will allow Medical Students to present a variety of audit and research work that have been undertaken across the country. The abstracts received were all very high quality.
Convenor: Sarah Stapley
Adjudicators: Simon Hodkinson, Sam Hook, Sarah Stapley, Sush Gowda, David Clarke, Dr Phil Harper, Dr Silva Allikmets, Rishi Das, Qamar Mustafa & Caroline Hing
09:00 - 09:05 Welcome & Introduction
09:00 - 12:30 Morning Session: Medical Student Abstracts (7 minute presentations with 2 minutes for questions)
Introduction: Sarah Stapley
09:05 - 09:14 Obesity does not adversely impact the outcome of unicompartmental knee arthroplasty for osteoarthritis: a meta-analysis of 80,798 subjects - Nikhil Agarwal
09:14 - 09:23 An analysis of national variance in coding for patellofemoral instability - Jatin Mistry
09:23 - 09:32 Diabesity is Associated with a Worse Functional Outcome and a Higher Risk of Superficial and Deep Wound Infection after Total Primary Hip Replacement - Jack Lovie
09:32 - 09:41 Intraoperative Communication is Associated with Lower Anxiety Levels in Fathers of Pediatric Patients undergoing Posterior Spinal Instrumentation and Fusion for Adolescent Idiopathic Scoliosis - Kevin Bondar
09:41 - 09:50 Crash Course in Orthopaedics: Lessons From a 12-Week Webinar Series for Medical Students - Catherine James
09:50 - 09:59 Epidemiology and long-term outcomes of lateral end clavicle fractures in an adolescent population - Rory Teed
09:59 - 10:08 Use of Pre-Operative EuroQol Five-Dimension (EQ-5D) to Prioritise Patients for Elective Hip and Knee Arthroplasty in the Aftermath of the COVID-19 Pandemic James Redmore
10:00 - 10:30 BREAK
10:30 - 10:39 Outcome comparison of Superior Capsule Reconstruction and Subacromial Balloon Spacers for the treatment of massive rotator cuff tears: A systematic review - Ciaran O'Hanlon
10:39 - 10:48 The Incidence of Major Complications Following Per-Acetabular Osteotomy (PAO) - Benjamin Rouse
10:48 - 10:57 Evaluation of Low-Intensity Pulsed Ultrasound usage and outcomes in bone healing- a retrospective audit - Rosalind Walsh
10:57 - 11:06 Intra-articular Steroid Injections and COVID19: Balancing the Risks and Rewards - Kira Faircloth
11:06 - 11:15 Determining key factors and predictors of 30-day mortality in pelvic ring fracture patients - Katya Qiao
11:15 - 11:24 Evaluating student perspectives on current orthopaedic teaching in undergraduate medicine - Ciaran O'Hanlon
11:24 - 11:33 The Effect of the use of Navigated and Manual Technology in Total Knee Replacements on Patient Reported Outcome Measurements Charlotte Jones
11:33 - 11:42 Delayed ACJ Reconstruction does not increase the risk of fixation failure or major complications - Hattie Pleasant
11:42 - 11:51 A robust treatment algorithm for pilon fractures: Our management and outcomes - Victor Lu
12:00 - 13:00
13:00 - 13:25 Introducing BOMSA
13:25 - 16:30 Afternoon Session: Practical Orthopaedics and Trauma Introduction and announcement of AM prizes
This session will allow medical student’s hands on sessions to undertake saw bone fixations of the ankle and wrist, apply an external fixator and utilise cement.
Round Robin sessions: Assisted by Stryker UK and Heraeus Medical
Participants can chose 4 of the 6 sessions to visit. Each will be timetabled for 30 minutes and be run 4 times according to demand.
Session 1: Ankle Fixation Presented by Zine Beech Consultant Orthopaedic Surgeon, University Hospital Southampton and Defence Medical Services
Session 2: Application of External Fixator Rishi Das (Trauma Fellow at St Mary’s and Imperial College and Mr Sush Gowda (Exeter Hip Fellow and Defence Medical Services)
Session 3: Using Cement Sam Hook Consultant Orthopaedic and Trauma Surgeon Portsmouth University Hospital Trust
Session 4: Locking versus non locking screws David Clark Consultant and Sarah Stapley
13:30 - 14:00 Practical Session 1
14:00 - 14:30 Practical Session 2
14:30 How to improve my chances of success into Higher Training Qamar Mustafa (ST3 Wessex Deanery)
15:00 - 15:15 Afternoon Break
15:15 - 15:45 Practical Session 3
15:45 - 16:15 Practical Session 4
16:15 Summing up and feedback session Sarah Stapley
16:30 End
Virtual Meeting the consultant: Running concurrently
Medical Students can book to speak with consultants
These will be run via zoom meetings. Accounts held by Sarah Stapley, Simon Hodkinson
Interviews will start at 13:30 and run for 15 minutes each. Participants will be provided with a zoom code to join.
08:30 - 16:00 Foot and Ankle Scotland (FASt)
Foot and Ankle Scotland (FASt) is a multidisciplinary group set up to provide an educational forum for Foot and Ankle Care across all disciplines in Scotland including Orthopaedic Surgeons, Podiatrists, Orthotists, Physiotherapists and other interested healthcare professionals involved in the provision of quality care for foot and ankle conditions.
Conference Suite 2B
Chairs: Nnamdi Obi, John McKinley, Bob Carter and Shariff Hazarika
Chair Free Papers: Sam Roberts
Speakers: Audrey Campbell, Sine Collins, Senthil Kumar, Shariff Hazarika, Natasha Rose, Mark Farndon and Lech Rymaszewski
Agenda:
08:30 Registration and coffee on arrival
09:15 Welcome to FASt Nnamdi Obi (FASt Chair)
Session 1 The Management of Neurological Conditions Affecting the Foot and Ankle John McKinley
09:20 - 09:35 Principles and strategies involved in neurorehabilitation Audrey Campbell
09:35 - 09:50 Orthotic approach to management Sine Collins
09:50 - 10:05 Surgical approach to management Senthil Kumar
10:05 - 10:10 Questions
Session 2 The Management of Talar Dome Osteochondral Lesions Bob Carter
10:30 - 10:50 Pathophysiology and evidence update Shariff Hazarika
10:50 - 11:10 Radiological modalities in the assessment of osteochondral lesions Dr Natasha Rose
11:10 - 11:30 Surgical approach to management Mark Farndon
11:30 - 12:00 Questions
Session 3 Experience and lessons learnt from Covid-19 in clinical practice Shariff Hazarika
13:00 - 13:15 Overview of board and departmental response to adaptation in clinical practice during Covid-19 Lech Rymaszewski
13:15 - 14:00 Open discussion
Session 4 Complex case discussion Nnamdi Obi
14:00 - 14:30 Complex cases
Session 5 Research Sam Roberts
14:30 - 15:30 Free paper session
08:30 - 12:00 Blended Training Orthopaedic Educational Supervisors (TOES)
Conference Suite 3
Chaired by: Lisa Hadfield-Law
Can you spare 8 hours to learn how to supervise trainees to be the very best they can? This Congress TOES programme will be blended. You will be required to work through the TOES learning log remotely and in your own time before the face-to-face live session at the BOA Congress in Aberdeen. We will open the programme on the 1st September with the learning logs sent to booked delegates via email, and run our face-to-face live session from 9am-12pm on Friday 24th September 2021 at Congress.
Please note before booking onto this TOES programme that the face-to-face session will not be recorded and booked participants will be required to attend in person at the BOA Congress in Aberdeen.
Learning Methods:
Most of the 8 hours of work required can be done remotely at a time convenient to suit you with just a 3 hour live session taking place face-to-face at the BOA Congress in Aberdeen.
1. Eliza Khalid will send a welcome briefing and learning log via email
2. Work through this at your own pace before the face-to-face live session at Congress
3. Facilitator reviews 1st 3 completed logs submitted to understand local issues
4. Once you have completed ALL modules you will swap with an allocated AES partner
Confirm that all modules are complete
Provide some written feedback in their partners learning log
Pass to the facilitator if there are any problems e.g. failure to complete
5. Facilitator will summarise how to handle the 3 trainee scenarios
13:30 - 15.00 IODA/WOW Webinar: Career breaks and how to bounce back (Virtual Session)
The International Orthopaedic Diversity Alliance (IODA) is honoured to co-host a free virtual symposium with the British Orthopaedic Association & Women in Orthopaedics Worldwide (WOW).
Register nowChaired by: Kristy Weber
Co-Chair: Camila De Mattos
Speakers: Deborah Eastwood, Zoe Little, Udo Anyaegie, Olof Lindén & Scarlett McNally
Agenda:
Challenging Change Deborah Eastwood (President-Elect BOA)
A return-to-work program for orthopaedics Zoë Little (UK)
Returning to work from parental leave Udo Anyaegie (Nigeria)
Returning to work from parental & research leave Olof Lindén (Sweden)
Returning to work after a health issue Scarlett McNally (UK)
Panel Discussion: Deborah Eastwood, Zoe Little, Udo Anyaehie, Olof Linden & Scarlett McNally
Should you have any queries please contact the BOA Events team at [email protected].
